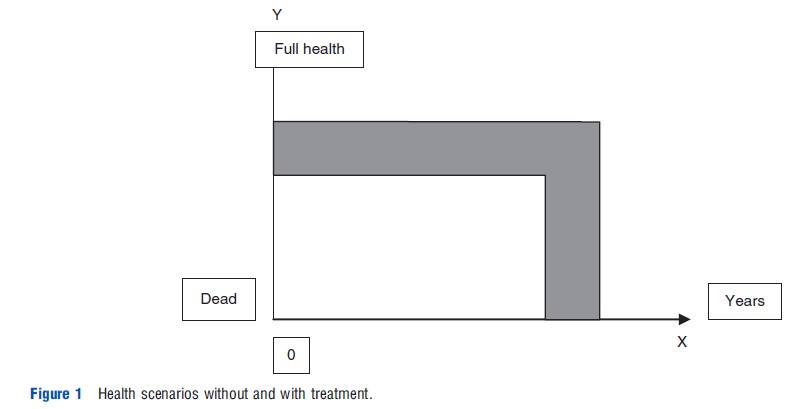
The quality-adjusted life-year (QALY) is a unit of measurement for valuing health outcomes. The background for it is illustrated in Figure 1.
In the diagram, length of life is expressed on the X-axis, whereas health status is expressed on the Y-axis on a continuum from dead to full health. The lower line shows the health of some hypothetical person over time with standard treatment. The upper line shows the health over time given some alternative better treatment. The total health gain from moving from standard to better treatment – represented by the area between the two lines – consists in gains both in level of health and length of life. The QALY is designed to capture in one single measure of value both these types of benefits so that they are made comparable and also may be added to each other. How this is done technically, is explained in the section Definition, Operationalization, and Meaning.
The value of an outcome measured in QALYs may be related to the cost of achieving the outcome. This is done in a so-called cost-effectiveness ratio (often called a cost-utility ratio). Cost-effectiveness ratios are indicators of value for money. Cost-effectiveness ratios using QALYs allow comparisons of value for money of different interventions in different areas of medicine – in which outcomes of different kinds are achieved – and may thus be an aid in priority setting and resource allocation decisions.
Definition, Operationalization, And Meaning
In the quality-adjusted life-years approach, 1 life year in full health for one person is used as a basic, reference outcome. For brevity, this is referred to as ‘1 well-year.’ One gained well-year is assigned a value of one QALY. The idea of the QALY approach is that any health outcome, whatever its nature and size, may be valued relative to the reference outcome, i.e., as equivalent to gaining some fraction of a well-year or some multiple of well-years.
Health outcomes that include gains or losses in quality of life are made comparable to outcomes consisting in gained well-years through the assignment of values to health states (Figure 2). The values on the Y-axis reflect the quality of life associated with the states – often called health-related quality of life. The values are on a scale from zero – corresponding to being dead or in a state as bad as being dead – to unity – corresponding to being in full health. They are used to weight life years in less than full health. For example, in Figure 2, state A is assigned a value of 0.8. Each gained life year in state A then yields 0.8 QALYs. This means that the gain is deemed equivalent to gaining 0.8 of a well-year.
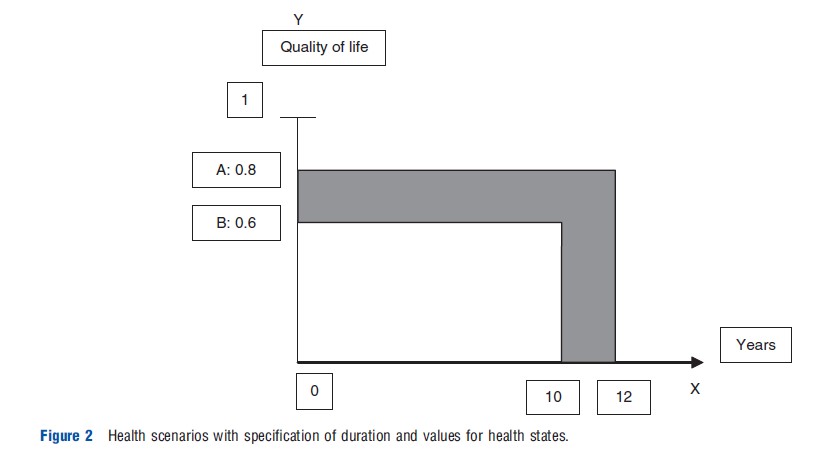
The number of QALYs in an individual’s health scenario over time is calculated by determining the value of each year in the scenario and summing these annual values over the whole time horizon. For example, if a person lives 3 years with values 0.8, 0.6, and 0.5 respectively, the value of the whole scenario is 0.8+0.6+0.5=1.9 QALYs. In Figure 2, 10 years gained in state B yields 6 QALYs (10×0.6), whereas 12 years in state A yields 9.6 QALYs. An improvement from state B to state A lasting 1 year yields 0.2 QALYs (0.8-0.6). If the improvement lasts 10 years, it yields 2 QALYs (10× 0.2) and is thus equivalent to 2 gained well-years. In Figure 2, the total value of replacing the first scenario with the second one is 10×0.2+2×0.8=3.6 QALYs.
Values and equivalence of health outcomes may be perceived and judged from different points of view. There is, for instance, a difference between pure self-interest of individuals and judgments of value by societal decision makers when concerns for distributive fairness are taken into account. Estimates of value in terms of QALYs are usually meant to express the personal value of outcomes to the recipients of the outcomes, without regard to distributive issues. Such personal value is commonly referred to as individual utility. An approach to valuing health outcomes from a broader societal perspective was outlined by Anthony Culyer and colleagues as early as in 1971 and later by for instance Erik Nord in 1992 and 1999.
To calculate the area under each curve in Figure 1 requires knowledge of the nature of the health states that are experienced, the sequence of these, the duration of each health state and the value of each health state. The former three kinds of knowledge require medical (clinical and/or epidemiological) data. Valuations of health states, on the other hand, is a psychometric task in which health economists have engaged heavily (together with researchers from other disciplines) with a view to making the QALY approach workable. Valuations are generally elicited from samples of the general population by means of one or more specially designed techniques for preference measurement, thereafter values are assigned based on mean or median responses.
Issues with Quality-Adjusted Life-Years
As noted above, estimates of value in terms of QALYs are usually meant to express personal value. Personal value is commonly referred to as individual utility. There are a number of methodological issues relating to the QALY approach as a way of estimating the individual utility of interventions.
First, health state utilities are usually obtained by asking representative samples of the general population to judge how bad it would be for them to be in different states of illness. This is referred to as decision utility. An alternative is to ask patients and disabled people to value the states they are in themselves. This would yield experience utility. Both approaches have strengths and weaknesses. As noted by Drummond et al. (2009), a widely held position in current health economics is that QALYs should be based on decision utilities elicited from people who are well informed about experience utility.
Second, for QALY-calculations to be meaningful and valid, utilities for health states need to have interval scale properties. That is, a change of a given size on the 0–1 value scale must have the same importance wherever it occurs on the scale. For instance, a move from 0.4 to 0.6 must have the same value as a move from 0.7 to 0.9. Techniques for preference elicitation vary with respect to their ability to yield utilities with interval scale properties.
Third, as noted above, the number of QALYs in a health scenario over time is calculated by determining the utility of each year in the scenario and summing these annual utilities over the whole time horizon. This means that the number of QALYs obtained from spending time in some fixed state is directly proportional to the length of that time. In other words, as noted by Bleichrodt et al. (1997) in a paper on ‘risk neutrality of life years,’ utility measured in terms of QALYs is (by definition) a linear function of length of time. In the real world, there is not necessarily a linear relationship between duration and utility. Individuals may, for instance, have diminishing marginal utility of length of life in the same way as they normally have diminishing marginal utility of goods and services. However, it is customary to discount QALYs in future years to take account of individuals’ preference for present consumption over future consumption. The number of discounted QALYs is less than proportional to the length of time in a state.
Fourth, in the QALY approach, each possible health state is associated with a single, fixed value. The value of a state is thus assumed to be constant across all individuals and contexts in which it may occur. Clearly, this single value convention is a simplification. Its rationale is a need to prevent valuation in terms of QALYs from becoming too demanding with respect to data and thus too complicated and time consuming. The convention is reasonable in many circumstances where QALYs are estimated in groups of people, in which cases individual deviations from standard health state values to a large extent cancel each other out. But the simplification does have some implausible implications that lead to continuous debates about the validity of QALYs. The most salient issues are noted below. Note that they all refer to valuations from a personal perspective. Some similar issues may be raised on grounds of concerns for fairness.
First, the single value convention means that the disutility of a state is considered to be independent of the gender, age, and other characteristics of the person who experiences the state, including the person’s attainable level of functioning. For instance, it means that dependence on eyeglasses or a walking stick is counted as equally bad for an elderly person as for an young person. It also means that inability to walk is counted as equally bad when it is occurs in a person with a longstanding incurable disability as when it is due to temporary, curable disease in a person who is normally in full health. These implications have been challenged on the grounds that most people have considerable capacity to adapt to and cope with durable disease and disability. This is particularly true of impairments resulting from normal ageing. So even if a person has health problems that people of medium age and normal health would regard as clearly undesirable, and if the person’s functional level is the best that he or she can reasonably hope for, his or her utility will not necessarily be much lower than that normally associated with full health. As noted by Erik Nord, Anja Enge, and Veronika Gundersen in 2012, this dependence of utility on what is to be expected and what one is used to may have important implications for valuations of gains in both length and quality of life in people with disability or chronic disease.
Second, the single value convention implies that the utility of a state to a person is considered to be independent of the person’s health in the past. For instance, if two people are dependent on eyeglasses, and one was blind in the preceding years, whereas the other had normal sight, the two will be assigned the same utility in their situation with eyeglasses. Concerns about this assumption led to a proposal by Mehrez and Gafni (1989) of an alternative to the QALY approach in which any scenario over time is valued as a whole instead of as a sum of independent valuations year by year. In the alternative approach, the unit of measurement is called the healthy year equivalent (HYE). The disadvantage of this approach is that valuation must be undertaken on all relevant sequences of health states, which may be numerous. Thus, there has been little use of the HYE approach in economic evaluation hitherto.
Third, the single value convention means that the value assigned to a health state does not depend on the duration over which the state is experienced. For instance, the utility of a state in the first year after the onset of a disability is the same as the utility of that state 5 years later even if the person in various ways may adapt to the state. At a more technical level, independence of duration further means that there are implicit assumptions of so-called mutual utility independence and constant proportional trade-off between quality of life and length of life when preference for health states are elicited.
Fourth, the single value convention means that the utility of a state is considered to be independent of its cause. For instance, the utility is the same for a congenital problem as for a problem caused by hospital negligence.
The concept of QALYs has been linked explicitly to expected utility theory. In a decision analytic framework, QALYs are used as the unit of account in expected value calculations for decisions under uncertainty. Expected utility theory dictates that in order for these expected value calculations to be consistent with preference over uncertain streams of health outcomes, QALYs should fulfill certain requirements of ‘utility’ functions. These requirements take the form of a set of axioms, formalized by von Neumann and Morgenstern in 1944. Although much has been written about empirical violations of the axioms of expected utility theory and various alternatives have been proposed, expected utility remains an important point of reference in many discussions of normative decision theory.
Several techniques are available for eliciting health state utilities from respondents, including the standard gamble, time trade-off, and the rating scale. Empirical studies have found that the different techniques produce values that differ systematically. Debates about the relative merits of the different methods refer both to economic theory and to comparisons of psychometric properties of the different measurement techniques.
It is clear from the points made above that the interpretation of health state values as estimates of individual utility in many ways is questionable. It is furthermore a fact that the second factor in QALY-calculations – the duration of health benefits – is purely a quantitative factor with no personal value judgments related to it. For instance, 10 years is simply counted as twice as much as 5 years, with no value judgment involved. Altogether, some therefore prefer to regard the results of QALY-calculations as indicators of the size of health effects rather than the utility – or personal value – of those effects. This alternative interpretation does not, however, alter the basic purpose of QALYs, which is to yield a quantitative estimate of efficiency in different areas of health care.
The QALY approach has been criticized on ethical grounds for implying priority to those individuals who have the greatest capacity to benefit from health care and for not taking into account concerns for fairness in the distribution of health care resources. Historically, the critique is understandable, given the primacy that cost-effectiveness ratios have been assigned in most of the health economics literature as guidance to priority setting. But a distinction needs to be made between calculations of QALYs and how the calculations are used in decision making. QALY estimates are essentially estimates of the aggregate individual utility of interventions. Although such information may be an important input in decision making about resource allocation, it does not follow that priorities should be set such that QALY gains are maximized as this may run counter to concerns for fairness such as wishes to give priority to the worse off and wishes to secure equal access to people in equal degree of need even if they are of different ages and/or have different potentials for health.
Historical Overview
Although the term QALY first appeared in the published literature in 1976, some earlier precedents may be found. Herbert Klarman and colleagues in 1968 compared three options for treating patients with chronic renal disease in terms of life years gained, with and without adjustments for ‘differential(s) in the quality of life.’ In 1970, Sol Fanshel and James Bush proposed measures of dysfunction-free years in evaluation of a tuberculin skin testing program. In 1971, Anthony Culyer and colleagues proposed a scheme for weighting life years within a social indicator framework. At the same time, George Torrance and colleagues introduced the index day and health day. Finally, the term quality-adjusted life-year was used in two separate publications in 1976, one by Milton Weinstein and William Stason examining policies for control of hypertension and another by Richard Zeckhauser and Donald Shepard in a more general exploration of analytic approaches to evaluating social policies with life-saving or health implications. An article by Weinstein and Stason appearing in the New England Journal of Medicine in the following year introduced QALYs to a broad medical and public health audience and is frequently cited as a major milestone in the development of cost-effectiveness analysis in health and medicine. In England, a highly influential early paper applying QALYs to evaluation of coronary artery bypass grafting was reported in an article by Williams (1985) in the British Medical Journal.
Researchers have developed a registry of cost-effectiveness studies that report outcomes specifically in terms of costs per QALY. Peter Neumann and colleagues reviewed the literature from 1976 through 2001 and identified 533 original studies meeting their inclusion criteria. Consistent with the earlier reviews of the broader cost-effectiveness literature, a major increase in the volume of studies on costs per QALY was evident, with 228 studies over the two decades from 1976 to 1997, followed by 305 studies over the 4-year period from 1998 through 2001.
Alternatives To Quality-Adjusted Life-Years
The disability adjusted life year (DALY) is a summary measure much like the QALY, developed by Christopher Murray and colleagues. The main difference is that it uses a scale of severity of illness from zero (full health) to unity (as bad as being dead) instead of a scale of utility from zero (dead) to unity (full health). The DALY was first developed for the primary purpose of quantifying the global burden of disease. However, the developers of the DALY explicitly intended that the measure could be used also as a metric for health benefits in the denominator of cost-effectiveness ratios. In the present day, the DALY is widely used – in fact much more than QALYs – in economic evaluation of health programs in developing countries.
The QALY procedure focuses on life years and the quality of these. In a paper in the British Medical Journal in 1992, Erik Nord argued that the health care system is concerned with providing care for people (‘living, breathing, feeling, and thinking individuals’), not with maximizing numbers of abstract time entities. The health care system is also concerned with meeting moral claims on treatment. The concept of claims is related to living subjects. Life years as such are not subjects and therefore do not have moral claims. Nord thus suggested the saved young life equivalent (SAVE) as an alternative to the QALY that focuses on persons rather than years. In the SAVE approach, the reference outcome consists in saving the life of a young person and restoring him or her to full health. The value assigned by society to this reference outcome is called a SAVE. In valuations that have a societal rather than an individual viewpoint, different kinds of health outcomes may all be valued relative to the SAVE, for instance using the so-called person trade-off technique. However, there has been little use of the SAVE in economic evaluation hitherto.
References:
- Bleichrodt, H., Wakker, P. and Johannesson, M. (1997). Characterizing QALYs by risk neutrality. Journal of Risk and Uncertainty 15, 107–114.
- Drummond, M., Brixner, D., Gold, M., et al. (2009). Toward a consensus on the QALY. Value in Health 12(Supplement), S31–S35.
- Mehrez, A. and Gafni, A. (1989). Quality-adjusted life years, utility-theory, and healthy-years equivalents. Medical Decision Making 9, 142–149.
- Williams, A. (1985). Economics of coronary artery bypass grafting. British Medical Journal 291, 326–329.
- Broome, J. (1993). QALYs. Journal of Public Economics 50, 149–167. Drummond, M. F., Sculpher, M., O’Brien, B., Stoddart, G. L. and Torrance, G. W.
- (eds.) (2005). Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press.
- Gold, M. R., Siegel, J. E., Russell, L. B. and Weinstein, M. C. (eds.) (1996). Cost-effectiveness in health and medicine. Oxford: Oxford University Press.
- Hauber, A. B. (2009). Healthy-years equivalent: Wounded but not yet dead. Expert Review of Pharmacoeconomics Outcomes Research 9, 265–269.
- Neumann, P. J., Greenberg, D., Olchanski, N. V., Stone, P. W. and Rosen, A. B. (2005). Growth and quality of the cost-utility literature, 1976-2001. Value in Health 8, 3–9.
- Nord, E. (1999). Cost-value analysis in health care: Making sense out of QALYs. Cambridge: Cambridge University Press.
- Nord, E., Daniels, N. and Kamlet, M. (2009). QALYs: Some challenges. Value in Health 12(Supplement), S10–S15.
- Richardson, J. (1994). Cost-utility analysis: What should be measured? Social Science & Medicine 39, 7–21.
- Weinstein, M., Torrance, G. and McGuire, A. (2009). QALYs: The basics. Value in Health 12(Supplement), S5–S9.