Health etymologically means being whole. Ancient philosophies describe health as a balance between qualities. Hippocrates’ view on health, as a balanced mixture of four humors, remained dominant till the sixteenth century. Aristotle stressed development of eudaimonia. From the sixteenth century the biomedical view emerged among physicians, whereas philosophers still stressed the larger context. The World Wars of the twentieth century stimulated the creation of international organizations on health, and the UN preparations led to the WHO. The minutes of these preparations express the idealism with which the WHO was established, as expressed in the WHO definition of health. The WHO aims at monitoring, so a family of classifications was designed, first mainly on diseases, later on functions. The WHO definition met criticism for its absoluteness and being static, and different definitions were proposed by physicians as well as philosophers. Three components are consistent in these proposals: capacity to perform, individual fulfillment, and relation to the social environment.
Etymology
Etymologically the English word ‘health’ means wholeness, being whole, complete, sound and well. To ‘heal’ literally means to make whole. Both words go back to the old English word ‘hal’ and the old German word ‘heil.’ The ancient Greek word for health was ‘euexia,’ which means to be in a good condition.
Historical Definitions of Health
Ever since human documentation existed, expressions are found where man differentiates between human states of well-being and ‘illnesses,’ the latter considered to be abnormal, undesirable and to be healed, if possible. In different ancient philosophies (e.g., Chinese, Indian, Egyptian, or Greek) concepts of illnesses and a state of ‘good health’ are described, and also the ways how man can achieve good health (Lindeboom, 1982). In these concepts, good health is conceptualized as a state of balance between different ‘elements,’ which represent different qualities, e.g., the five elements (wood, fire, earth, metal, and water) and the Yin and Yang qualities in Chinese philosophy (Taoism), or the four humors in Greek medicine (black and yellow bile, phlegm, and blood), which originated from knowledge of ancient Egypt and Mesopotamia.
Health is described to be achievable and influenced by lifestyle habits and in certain circumstances, if fate allows, to be influenced by god(s), as mediated by priests in temples. ‘Hygeia’ was the name of the goddess of health in ancient Greece, the daughter of Asclepius, who represented a good way of living.
Physicians and Philosophers
Over the course of history, physicians as well as philosophers have developed views on the nature of health. Hippocrates (approximately 460–370 BC) (London, 1984), is still considered to be ‘the father of Western medicine,’ as he was the first to emphasize the importance of a good physical examination of the patient; he created a new paradigm, discriminating in humans four humors: black bile (melan chole), yellow bile (chole), phlegm (phlegma), and blood (haima), each corresponding to one of the traditional four elements and temperaments. A healthy situation was the balance between the four humors, and Hippocrates considered diet to be the most influential lifestyle factor in changing the relative proportions between the four, in addition to influences from climate, winds, quality of the water, and the soil.
Historically even more influential Greek-Roman doctor Galen (131–216) followed and refined the teachings of Hippocrates and described six lifestyle factors, ‘res non naturalia,’ which should be in balance in order to maintain health: food and drink (cibus et potus), sleep and being awake (somnus et vigilia), light and air (aer), secretions and excretions (secreta et excreta), work and relaxation (motus et quies), and emotions (affectus animi).
The ‘father of Western philosophy,’ Aristotle (384–322 BC) does not discuss ‘health’ as such, but states that extremes in bodily condition should be avoided and maintaining a proper balance (the mean) is a virtue (Osborne, 2011). Yet, in his ethics he considers ‘eudaimonia’ or well-being to be the final goal and good for man. Eudaimonia is an important concept as it is rediscovered in modern views on health. Eudaimonia literally means ‘the state of having a good indwelling spirit, a good genius’; in modern translations, it is described as ‘happiness’ or ‘personal well-being.’ Eudaimonia is not a static state but a continuous process of development, to fulfill one’s potentials and to flourish. This implies self-realization, by which man achieves this happiness and personal well-being.
These views of Hippocrates, Galen, and Aristotle, about the human potential to be in a state of balance and the virtue of developing oneself, remained highly influential in Western medicine and thinking over fifteen centuries.
From the Sixteenth Century – A New Paradigm Dawns in Medicine
The Physicians’ View
A different way of interpreting human health and disease started emerging in medicine when Vesalius (1543) published his studies on the anatomy of the human body. These were based on his own observations by the dissection of bodies, which was considered sacrilege until then. A century later William Harvey (1628) described the system of blood circulation, which was until then thought to be a tidal movement, like ebb and flow. The Galenic humoralism was definitely displaced in 1858, when Rudolph Virchow published his theory on cellular pathology (Virchow, 1858, 1862). In the same period, Semmelweiss discovered the protective effect of disinfective measures against deathly puerperal fever; soon thereafter Pasteur described the existence of bacteria, which he could see in the microscope, and the ways to disarm these (e.g., by pasteurization). From then the paradigms of cell physiology, microbiology, and pathological anatomy became the dominant views in medicine. Diseases were no longer understood as caused by misbalances of qualities, but were to be searched and understood in the physical body, in organs, in cells and in microbes, and should be treated there. Health became the absence of disease (Shorter, 2009).
Parallel to this transition in medical thinking, public health developed in the fast growing cities due to the industrial revolution and by sanitary measures, clean water provision, garbage disposal as well as first vaccinations, infectious diseases like cholera, typhus, and small pox were eradicated and became extinct. The new medical paradigm proved to be effective.
Contemporary Philosophers in the Eighteenth and Nineteenth Century
In the period of this paradigm shift in medical thinking, philosophers still had a broader perspective on health, than as absence of disease. From Goethe (1749–1832) comes the quote “What is the highest virtue on earth? To be healthy? No: to become healthy” (Hygiene Museum Dresden). Nietzsche (1844–1900) discriminated between ‘small health’ and ‘big health’ (Verduin, 1998). While ‘small health’ in his view is concerned with the daily derangements and illnesses with which doctors deal, attaining ‘big health’ means saying a full YES toward life, with all its insecurities, tragedies and finally death. Big health includes small health, but is connected to growth far beyond that.
Health in the Twentieth Century and the Foundation of the WHO
From the twentieth century, public health started to be organized on a national and international scale, operated by big health organizations (Borowy, 1988). In 1902, the Pan American (international) Sanitary Bureau was founded in Washington DC, while in 1907 the Office International d’Hygiène Publique followed, with headquarters in Paris. In 1913, the Rockefeller Foundation as a first nongovernmental organization was initiated with the aim to enhance the well-being of all mankind.
After World War I, the League of Nations Health Organisation was established, which stood out as the first official body with a global perspective and the broadest work spectrum. In 1919, the League of Red Cross Societies was organized, which developed health programs with an international outlook.
In 1943, a Health Division of the United Nations Relief and Rehabilitation Administration was initiated by the U.S. President Roosevelt “for the relief of victims of war in any area under the control of any of the United Nations through the provision of food, fuel, clothing, shelter and other basic necessities, medical and other essential services.” The term ‘United Nations’ referred to the Allies of World War II.
World War II led to the wish to establish a world organization like the present United Nations, to preserve world peace toward the future. When in 1945 in San Francisco 50 nations met to draft the Charter of the future United Nations, among them there were three medical doctors from Norway, Brazil, and China. They met 1 day for a ‘medical lunch,’ where the Norwegian Karl Evang suggested “Why don’t we start a new health organization?” (WHO, 1988). The idea was to unite the different existing organizations in one single health organization. The men succeeded in having the word ‘health’ inserted in the Charter of the United Nations and they recommended the general conference to establish an international health organization. This was approved unanimously and this was the very beginning in 1945 of the WHO.
A Technical Preparatory Committee was established to prepare a draft Constitution of the WHO. This committee of 16 men and advisors met in Paris 22 times between March and June 1946. Their work resulted in the draft Constitution of the WHO, which was signed on 22 July 1946 by the representatives of 61 states at the International Health Conference in New York. Thereafter all countries had to ratify the Constitution, which was completed in 1948.
Between 1946 and 1948, an Interim Committee, presided by Andrija Stampar from Yugoslavia, ensured continuity. This Committee decided in favor of Geneva as seat for the headquarters of the WHO, and it was in Geneva at the first World Health Assembly that the Constitution entered into force on 7 April 1948.
The Constitution of the WHO
The Constitution of the WHO starts with the Preamble, stating the principles upon which the whole document is based (WHO, 1948):
The States parties to this Constitution declare, in conformity with the Charter of the United Nations, that the following principles are basic to the happiness, harmonious relations and security of all peoples:
Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.
The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition.
The health of all peoples is fundamental to the attainment of peace and security and is dependent upon the fullest co-operation of individuals and States.
… Etcetera.
The definition of health has a central position in the Preamble Constitution of the WHO. There had been some discussion whether a definition of health should be in the Constitution. Szeming Sze, a public health doctor from China, one of the three who initiated the idea for the WHO and a member of the Technical Preparatory Committee, describes how the phrasing of the definition of health came about (WHO, 1988). Some detail on this process is also to be found in the minutes of the Technical Preparatory Committee (WHO, 1947). A subcommittee of four physicians, Canadian psychiatrist Brock Chisholm (later to become the first Director-General), Argentinian psychiatrist Gregorio Bermann, Joseph Cancik from Czechoslovakia, and Sze himself had ‘some pleasant academic discussions’ and decided to emphasize mental health as well as the preventive side of health and so they came to the wording of health as not merely the absence of disease. The minutes of the Technical Preparatory Committee describe several preversions of the definition, with terms like ‘physical fitness’ and ‘positive health.’
Idealistic Intentions
The WHO definition of health is, like the Constitution as a whole, phrased very idealistically. One should realize these are formulated in a reaction to the horrors of World War II. The atmosphere in the Preparatory Committee may be characterized by a phrase in the minutes of this Committee where Chisholm is cited with the following phrase: “The world was sick, and the ills from which it was suffering were mainly due to the perversion of man, his inability to live at peace with himself. It was in man himself that the cause of present evils should be sought. The microbe was no longer the main enemy: science was sufficiently advanced to be able to cope with it admirably, if it were not for such barriers as superstition, ignorance, religious intolerance, misery and poverty. These psychological evils must be understood in order that a remedy might be prescribed, and the scope of the task before the Committee, therefore, knew no bounds. For that reason Dr. Chisholm associated himself with the ‘visionaries.’ What was taking place in these meetings would be of great historical importance if all members aimed at universal and worldwide achievement. To do this, they might find it necessary to bite off more than they could chew, but the alternative was complete chaos. They should do their utmost to bring all the peoples of the world together in the service of physical, social and emotional health.”
Chisholm refers to penicillin, which became available for general use, after Fleming had discovered it in 1928. In a time where infectious diseases were still dominant, this discovery nourished great expectations to ban these diseases. Yet, the broadness of the definition of health, beyond the absence of disease, was at the time ground breaking and is owed to this special group of physicians, who directed this process of establishment.
In several charters, declarations and statements the idealistic aims of the WHO were renewed every few years since the inception of the definition of health, (http://www.who.int/healthpromotion/conferences/en/). Of these, the best known is the ‘Alma Ata Declaration,’ which emerged from the UNICEF/WHO Conference on Primary Health Care of 1978, addressing health as a fundamental human right, health inequalities and the connected need for economic and social development; the ‘Health for All by the year 2000’ declaration of 1981, as target for the WHO; and especially the condensed and strongly formulated ‘Ottawa Charter for Health Promotion’ of 1986. There the WHO definition was described in connection to the conditions by which this state could bemet: “To reach a state of complete physical mental and social well-being, an individual or group must be able to identify and to realize aspirations, to satisfy needs, and to change or cope with the environment. Health is, therefore, seen as a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities. Therefore, health promotion is not just the responsibility of the health sector, but goes beyond healthy lifestyles to well-being.” As fundamental “prerequisites for Health are mentioned: peace, shelter, education, food, income, a stable co-system, sustainable resources, social justice and equity.” The charter calls for ‘building healthy public policy’ and the ‘creation of supportive environments.’
During the 2013, Helsinki 8th Global Conference on Health Promotion the tone was a somewhat less idealistic and the ‘implementation gap’ was addressed. It was concluded that the ‘Health in All Policies’ approach was one of the key domains of shared governance toward health in the twenty-first century. In all these texts, the original definition of health of the WHO was maintained.
Operationalization of Health by the WHO since 1948
The WHO Classification Systems
The WHO intends to monitor population health around the world and is thus in need of health indicators (Chatterji et al., 2002). Yet, the WHO itself recognizes that the definition is not sufficient to develop operational indicators of health. The definition places health in the broad context of well-being in general, whereas health in itself is separate of well-being, yet instrumental for it. Health is first of all an attribute of an individual person and comprises states or conditions of the human body and mind; attempts to measure health must thus include measures of functions of body and mind.
There is general acceptance of describing health states of individuals, in terms of multiple domains and in self-report instruments. For measurement purposes of health status valid, reliable, and comparable indicators are needed. According to the WHO, a measurement instrument requires:
- a classification of health status domains,
- specification of a set of domains necessary and sufficient to describe health states for measurement purposes,
- specification of what is being measured in each domain,
- a common understanding of what is full health versus exceptional talent in any given domain, and
- if it is required, to construct summary measures of average level of population health, a method to place a single cardinal value on the overall level of health associated with a health state defined on multiple domains (Chatterji et al., 2002).
Since 1948, the WHO designed several classification systems, together described as the WHO Family of International Classifications (http://www.who.int/classifications/en/). At first, the focus was on causes of mortality, diagnoses, and causes for morbidity, for which the International Classification of Diseases (ICD) and Related Health Problems was developed, which is the international standard for epidemiological purposes.
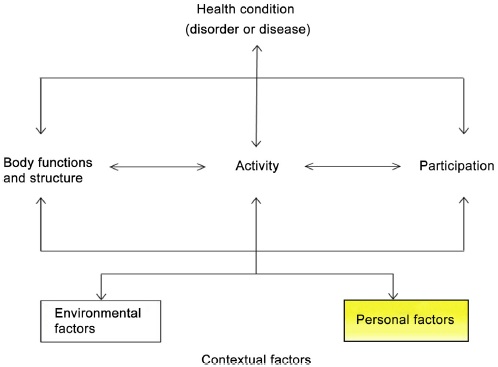
However, gradually thinking about health states evolved and in order not to just evaluate mortality and diseases, but also disabilities, functioning and health states, the International Classification of Functioning, Disability and Health (ICF) (previously the International Classification of Impairments, Disabilities and Handicaps (ICIDH)) was elaborated (Figure 1). The ICF measures six domains of activity and participation, by a person’s capacity, as well as performance. The gap between capacity and performance is considered to reflect the impact of the actual environment. The ICF goes beyond health condition, functions, activity and participation, and also takes environmental factors into consideration. The domain of personal factors is least elaborated, in fear of ‘blaming the victim,’ e.g., in cases of health damage through inequalities.
Figure 1. The different domains, included in the international classification of functioning, disability and health.
Quality of Life and Well-Being and Health-Related Quality of Life
Objective indicators of health and functioning as specified in the ICF need to be distinguished from a person’s subjective appraisal of well-being and quality of life (QoL). It can very well be that a person with impairments still experiences a good QoL; this is called the ‘disability paradox’ (Faber von et al., 2001). In this context, the WHO identifies ‘QoL’ as “an individual’s perception of their position in life in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards, and concerns” (Chatterji et al., 2002).
The WHO developed several instruments for measuring well-being and QoL: the WHOQoL-100 (http://www.who.int/mental_health/en/) with 100 items covering six domains and the WHOQoL-BREF (http://www.who.int/substance_abuse/en/) with 26 questions in four domains, which are worldwide one of the most widely used instruments for assessing QoL. The short WHO-5 well-being index (http://www.sayhelp.net/) connects wellbeing mainly to mental health.
General QoL should be distinguished from Health-related QoL (HR-QoL), i.e., QoL perceived in relation to symptoms, impairments, and functions.
For HR-QoL, the best-known measurement instruments (from outside the WHO) are the SF-36, the Health Utility Index (HUI), the Nottingham Health Profile (NHP), and the EQ-5D.
Many more measurement approaches have been developed, like the measurement of QALY’s (Quality-adjusted Life Years) or DALY’s (Disability-adjusted Life Years), but these will not be described here.
Contemporary Philosophers of the Twentieth and Twenty-First Century on Health
The WHO was designed and further developed mainly by members of the medical profession. Yet ‘health’ is not a topic that concerns just physicians – it concerns humanity as a whole and during the existence of the WHO also philosophers have thought about health. Some influential views should be mentioned.
In 1975, Christopher Boorse presented his Bio-Statistical Theory (BST) (Boorse, 1975, 1977), theorizing that ‘health’ is a state within a range of species typical normal functioning and thresholds in the organism; consequently disease is abnormal functioning. Health is thus the absence of disease, with a strict demarcation. Normal functions can empirically and statistically be discovered by the natural sciences and are thus objective and value-free, according to Boorse. The need is to develop enough and appropriate reference classes, connected to functions. Despite diverse criticism, the appeal to reference classes is commonly accepted in health care and the theory reached the status of background theory of health and medicine (Venkatapuram, 2013).
Out of discontentment with the prevailing view of health as the absence of disease, the Swedish philosopher Lennart Nordenfelt published in 1987 (revised in 1995) his theory of ‘health as the ability to achieve vital goals.’ Nordenfelt described a person’s vital goal as “a state of affairs that is such that it is a necessary condition for the person’s minimal happiness in the long run.” The stipulation ‘in the long run’ is aimed at avoiding the definition of health to be centered on immediate pleasure and instead, be more in line with long-term happiness, thriving, or flourishing such as Aristotle’s eudaimonia. More recently (1995), he rephrased the definition of vital goals as “a state of affairs which is either a component of or otherwise necessary for the person’s living a minimally decent life. This includes more than survival” (Nordenfelt, 2001; Venkatapuram, 2013).
In 2013, Venkatapuram proposed a modification of Nordenfelt’s concept of health (Venkatapuram, 2013). He criticizes Nordenfelt’s definition in that it conceptualizes vital goals as social, cultural and ethically relative and, thus, subjective and not normative; in addition, Nordenfelt does not specify a set of vital goals. Venkatapuram aims to describe a human species-wide conception of basic vital goals or ‘central human capabilities and functionings,’ as inspired by the capabilities approach of Martha Nussbaum, which sets a norm.
Venkatapuram reasons that ‘health is a person’s ability to achieve or exercise a cluster of basic human activities.’ He refers to Nussbaum’s 10 capabilities, which consist in a life worthy of human dignity: (1) being able to live a normal length of life span; (2) having good health; (3) maintain bodily integrity; (4) being able to use senses, imagination, and think; (5) having emotions and emotional attachments; (6) possess practical reason to form a conception of the good; (7) have social affiliations that are meaningful and respectful; (8) express concern for other species; (9) able to play; and (10) have control over one’s material and political environment.
Venkatapuram stresses that these 10 capabilities, as moral entitlements emanating from a person’s human dignity, become the source of political principles for a liberal pluralistic society; ensuring that each member achieves a threshold level of these 10 central capabilities become primary political goals. He expects different societies to define thresholds levels of each capability depending on their history and resources, and thus defining health as a minimal conception of human well-being (Venkatapuram, 2013).
A clear ethical statement is being made, which in its intention is similar to the ideals of the WHO. It is remarkable that a philosophy such as the one by Boorse reaches the medical establishment, whereas the philosophies of Nordenfelt and Venkatapuram do not cross the apparent gap between philosophy and medicine. Or are new developments promising for more exchange and integration?
More Health Concepts Outside the WHO in the Twentieth and Twenty-First Century
In the twentieth and twenty-first centuries also nonphilosophical professionals outside the WHO thought about the definition of health, some of whom are mentioned here.
In 1941 Henry Sigerist, a Swiss born American medical historian, analyzing the relevance of health for human welfare, stated that “A healthy individual is a man who is well balanced bodily and mentally, and well-adjusted to his physical and social environment. He is in full control of his physical and mental faculties, can adapt to environmental changes, so long as they do not exceed normal limits, and contributes to the welfare of society according to his ability. Health therefore is not simply the absence of disease; it is something positive, a joyful attitude towards life, and a cheerful acceptance of the responsibilities that life puts upon the individual” (Sigerist, 1941).
René Dubos, a French-born American microbiologist and humanist (well known by his ‘Think global, act local’) stated in 1968 that in his view “Health is a modus vivendi enabling imperfect men to achieve a rewarding and not too painful existence while they cope with an imperfect world. Health and vigour can be achieved in the absence of modern sanitation and without the help of Western medicine. Man has in his nature the potentiality to reach a high level of physical and mental well-being without nutritional abundance or physical comfort” (Dubos, 1968).
Ivan Illich, Austrian philosopher, Roman Catholic priest and critic of the institutions of contemporary Western culture, described health in 1975 as “the ability to adapt to a changing environment, to growing up and to aging, to healing when damaged, to suffering and to the peaceful expectation of death. Health embraces the future as well, and therefore includes anguish and the inner resources to live with it” (Illich, 1975).
Stokes, Noren, and Shindell described in 1982 health as “A state characterized by anatomical, physiological, and psychological integrity; an ability to perform personally valued family, work, and community roles; an ability to deal with physical, biological, and psychological stress; a feeling of well-being; and freedom from the risk of disease and untimely death” (Stokes et al., 1982).
In 1995 Last described health as “A state of equilibrium between humans and the physical, biological, and social environment, compatible with full functional activity” (Last, 1997).
In 1996, Tarlov analyzed the definitions of health of the past half century and concluded that there is a remarkable consistency of three conceptual components, being:
- The capacity to perform (relative to potential).
- The achievement of individual fulfillment; the pursuit of values, tasks, needs, aspirations, and potential.
- In a social environment, good health provides the potential to negotiate demands of the social environment.
Salutogenesis
In addition to these definitions of health, the American-Israeli medical sociologist Aaron Antonovsky introduced in 1979 a new term on health, which he called salutogenesis (Antonovsky, 1979), i.e., the study of generating health, as opposed to pathogenesis, the study of diseases. Antonovsky found during his qualitative studies in Israel that a certain group of women, who had survived concentration camps, did not have negative health outcomes in response to their experiences and could manage stress and stay well. Apparently, some people achieve health despite their exposure to potentially disabling stress factors. Antonovsky studied the characteristics of these resilient people and found three personality traits, which in combination he called the Sense of Coherence (SOC).
SOC consists of comprehensibility, manageability, and meaningfulness. Antonovsky described meaningfulness to be the strongest factor. The importance of meaningfulness is in concordance with the findings of psychiatrist Viktor Frankl, based on his own observations among survivors of concentration camps (Frankl, 2006).
SOC reflects two of the three previously described components in Tarlov’s analysis of definitions of health: The component of capacity to perform reflects manageability, whereas the achievement of individual fulfillment reflects meaningfulness. Where Antonovsky adds comprehensibility, Tarlov describes the importance of the social environment.
Antonovsky rejects the view of health and disease as sheer opposites; rather he describes the two as extremes on a continuum and stresses the possibilities to strengthen SOC, in order to enhance health. His views are further elaborated, among others, by Lindström and Eriksson (2010).
Increasing Criticism of the WHO Definition of Health in the Twenty-First Century
In 2008, Alex Jadad from Canada initiated a global conversation using a Web-based discussion forum (blog) for which he invited participants in the British Medical Journal (Jadad, 2008). This blog was like a reenactment of the discussion of 60 years ago, which led to the WHO definition, with the major difference of using the power of social media. Shortly thereafter, an editorial published in The Lancet was entitled ‘What is health? The ability to adapt’ (Lancet, 2009).
At that time in the Netherlands also the urgency was felt for redefining health in a more dynamic and operational way. At the end of 2009, a 2-day international expert conference was organized about ‘health.’ First limitations of the WHO definition were discussed and summarized as follows: (1) the absoluteness of the word ‘complete,’ which is utopian and stimulates medicalization; (2) the present demography of diseases, which shows no longer infectious, but mainly chronic diseases; and (3) the difficulty with operationalization, as ‘complete’ is not measurable. There was broad support for moving from the present static formulation of the WHO definition of health, toward a more dynamic description based on resilience and the human capacity to cope and to maintain and restore one’s integrity, equilibrium, and sense of well-being.
Participants questioned whether a new formulation should be called a definition, because this implies set boundaries and trying to arrive at a precise meaning. They preferred the definition should be replaced by a concept or conceptual framework of health. A general concept, according to sociologist Blumer, represents the characterization of a generally agreed direction in which to look, as a reference. But operational definitions are also needed for practical life, such as for measurement purposes. The preferred description for a dynamic general concept was “Health as the ability to adapt and to self-manage, in the face of social, physical, and emotional challenges.” This was published in the British Medical Journal (Huber et al., 2011).
In 2012–13, this general concept was further elaborated by Huber into the broad operational concept of ‘positive health,’ integrating objective medical and functional facts on the one hand, and SOC and meaningfulness on the other hand, thus approaching the ideals of Nordenfelt and Venkatapuram, and presenting optional concepts for ‘personal factors’ in the ICF. At present, (2014) a scientific publication is in preparation.
Bibliography:
- Antonovsky, A., 1979. Health, Stress and Coping. Jossey-Bass Publishers, San Francisco, ISBN 978-0-671-02337-9.
- Boorse, C., 1975. On the distinction between disease and illness. Philosophy & Public Affairs 5, 49–68.
- Boorse, C., 1977. Health as a theoretical concept. Philosophy of Science 44, 542–573.
- Borowy, I., 1988. The league of nations health organization: from European to global health concerns? In: Andresen, A., Hubbard, W., Ryymin, T. (Eds.), International and Local Approaches to Health and Health Care. University of Bergen 2010, pp. 11–30.
- Chatterji, S., Ustün, B.L., Sadana, R., et al., 2002. The conceptual basis for measuring and reporting on health. WHO. In: Global Programme on Evidence for Health Policy Discussion Paper No. 45.
- Dubos, R., 1968. Man, Medicine, and Environment. Praeger, New York, p. 69.
- Faber von, M., Bootsma-van der Wiel, A., van Exel, E., et al., 2001. Successful aging in the oldest old: who can be characterized as successfully aged? Archives of Internal Medicine 161, 2694–2700.
- Frankl, V., 2006. Man’s Search for Meaning, Part One, ‘Experiences in a Concentration Camp’. Pocket Books, ISBN 978-0-671-02337-9.
- Goethe; quote on glass plate at the entrance of the Hygiene Museum in Dresden. Harvey, W., 1628. De motu cordis. Level 12 Spec Coll Hunterian Ac.4.18, Frankfurt.
- Hippocrates, 1984. Nature of Man. Humours. Aphorisms, vol. IV. Loeb Classical Library, No 150, London.
- Huber, M., Knottnerus, J.A., Green, L., et al., 2011. How should we define health? British Medical Journal 343, d4163.
- Illich, I., 1975. Medical Nemesis: The Expropriation of Health. Marion Boyars, London, p. 167.
- Jadad, A.R., 2008. How should health be defined? British Medical Journal 337 (a2900), 1361–1364.
- The Lancet 373 (9666), 7 March 2009, 781.
- Last, J.M., 1997. Public Health and Human Ecology. Conn. Appleton & Lange, Stanford.
- Lindeboom, G.A., 1982. Begrippen in de Geneeskunde. Editions Rodopi, Amsterdam, 33–41.
- Lindström, B., Eriksson, M., 2010. The Hitchhiker’s Guide to Salutogenesis. Salutogenic Pathways to Health Promotion. Folkhälsan, Helsinki.
- Nordenfelt, L., 1995. On the Nature of Health: An Action-Theoretic Approach, second ed. Kluwer Academic, Dordrecht.
- Nordenfelt, L., et al., 2001. Health, Science, and Ordinary Language. Rodopi, Amsterdam.
- Osborne, R., 2011. The History Written on the Classical Greek Body. Cambridge University Press, Cambridge, New York.
- Shorter, E., 2009. Doctors and Their Patients, a Social History, sixth ed. Transaction Publishers, New Brunswick, NJ.
- Sigerist, H.E., 1941. Medicine and Human Welfare. Yale University Press, New Haven.
- Stokes, J., Noren, J.J., Shindell, S., 1982. Definition of terms and concepts applicable to clinical preventive medicine. Journal of Community Health 8, 33–41.
- Tarlov, A.R., 1996. Social determinants of health: the sociobiological translation. In: Blane, D., Brunner, E., Wilkinson, R. (Eds.), Health and Social Organization. Routledge, New York, pp. 71–93.
- Venkatapuram, S., 2013. Health, vital goals, and central human capabilities. Bioethics 27 (5), 271–279.
- Verduin, P., 1998. Thesis: De vraag naar het lichaam. Elsevier/De Tijdstroom, 25–35.
- Vesalius, A., 1543. De humani corporis fabrica libri septem, Basel Level 12 Spec Coll Hunterian Z.1.8.
- Virchow, R., 1858. Vorlesungen über Pathologie. A. Hirschwald, Berlin.
- Virchow, R., 1862. Die Cellularpathologie in ihrer Begründung auf physiologische und pathologische Gewebelehre. A. Hirschwald, Berlin.
- WHO, 1947. Minutes of the Technical Preparatory Committee for the International Health Conference Held in Paris from 18 March to 5 April 1946. Citation Chisholm, p. 13.
- WHO, 1948. http://www.who.int/governance/eb/who_constitution_en.pdf
- WHO, 1988. From small beginnings. Interview with szeming sze. World Health Forum 9.