Rapid increases in overweight and obesity prevalence rates over the last few decades, accompanied (and caused) by widespread dietary imbalances, are imposing huge burdens on health care systems and reducing the quality of life of populations around the world. These trends are not limited to the developed world alone, where there is talk of an ‘obesity epidemic,’ but also apply to several developing, transition, and middle-income countries. Between 1991 and 2008, the obesity prevalence rate in the UK grew from 14% to 25.4%, whereas in the US the percentage of obese individuals rose from 23.3% to 35.4%. Several countries undergoing economic transition have also witnessed a parallel ‘nutrition transition,’ characterized by significant increases in energy density, fat, sugar and salt content of local diets, and spiraling rates of overweight and obesity prevalence and associated disease costs. For example, 77% of Mexican men and 66% of women are now overweight, and Mexico is in the top tier of countries in obesity league tables.
In this article, the authors discuss the main macroeconomic causes and consequences of poor diets, obesity, and associated noncommunicable disease. The counterfactual implications of a movement toward better diets, and policy measures available to governments to improve diets are also discussed. Attention is restricted to the aggregate level – sector, economy, or population-wide issues – with microeconomic, individual/household level issues discussed only when relevant to the aggregate picture (government policies, applicable at the population level, are considered macro even if they work by affecting incentives at an individual level).
Causes
The debate about the attribution of obesity to economic factors has grown along with obesity rates in developed countries. A variety of factors – including genetic, psychological, and social drivers – have been put forward as potential causes. These are all relevant in explaining heterogeneity in weight within a cross section of people, but are consistent only to a limited extent with the speed of observed rise in the overall proportion of overweight and obese individuals over the last two decades. Because rapid changes are more likely to be rooted in socioeconomic factors, the role of economics in explaining the so-called obesity epidemic has gained prominence. Weight change is a function of the difference between calorie intake change and energy expenditure (physical activity) change (although some researchers also attribute a role to diet quality, for example, proportion of energy sourced from fat). Estimates of average daily per capita calorie intakes over the period 1991–2007 show a 7.8% increase for the UK, a 6.8% increase for the US (and a 9.9% increase for developing countries, although in their case a proportion of this is a welcome improvement to the calorie intakes of the undernourished). The US has also experienced a substantial rise in fat intake (+14.1%). Economic drivers are seen as fundamental to these changes.
Technological Change And Commodity Prices
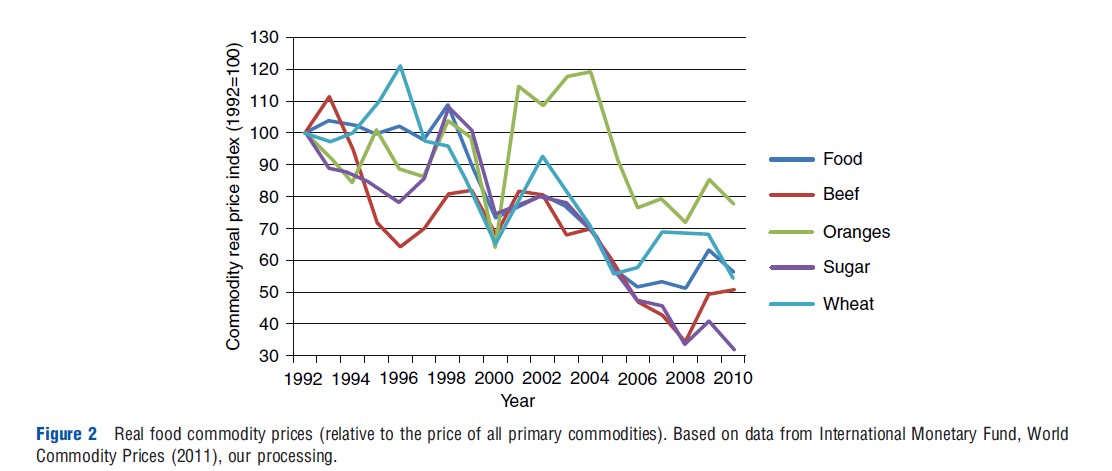
The argument that has gained most consensus in explaining the growth in obesity rates is related to the impact of technological change. Technical progress has rapidly increased agricultural productivity and lowered the cost of food. Furthermore, this trend has been uneven across foods, as the relative price of industrial and processed foods (and raw inputs like sugar) has declined at a faster pace compared to raw foods like fruits and vegetables. Figure 1 shows how productivity in the cereal sector has sharply risen over the last two decades, even in countries like the UK (+15%) and the US (+47%), where yields were already very high and much higher than the world average (+29%).
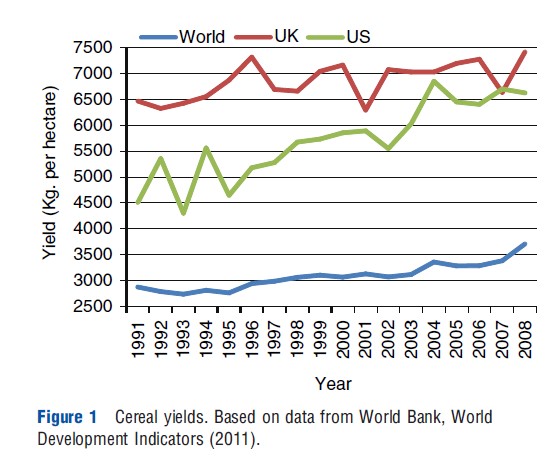
The sharp decline in real commodity prices shown in Figure 2, together with the relatively small but regular increase in incomes, has contributed to the rise in calorie intakes observed in developed countries. In developing countries – especially in transition countries where income growth has been much more substantial – the effect on calorie intakes is even stronger, which explains why many of these countries are now experiencing rapidly rising obesity rates while still being affected by food insecurity. Technological change also matters to the other term in the weight change equation, calorie expenditure, and this effect is possibly even more influential than commodity price decline or income growth. There is strong evidence that jobs have become much more sedentary, and that physical activity has been transferred from paid working time to costly leisure time.
In summary, technological change has made calorie consumption progressively cheaper, whereas raising the costs (including time costs) of calorie expenditure.
Food Availability And Globalization
On the supply-side, particularly in developed countries, the increased availability of ‘junk food,’ defined as calorie-dense foods high in fats, sugar and salt has been also blamed (in developing and transition countries, increased livestock product consumption has similarly been blamed). From an economist’s perspective, unless one accepts the asymmetric information assumption or some sort of oligopoly due to market segmentation, an increase in production of junk foods can be explained either by higher profitability for the industry or by the increased consumer demand. The former explanation can be traced back to the technological change hypothesis, as processing of commodities into energy-dense packaged foods has become cheaper over time. Growing demand (and consumption) would reflect changing preference toward these foods compared to healthier dietary options, but no data exists to test this hypothesis over time.
Increased globalization and trade openness have played an important part, particularly in many developing countries. This is partly considered a cultural (demand-side) effect, sometimes called ‘coca-colonization,’ wherein unhealthy dietary patterns first established in developed countries are emulated by developing country consumers, with increased globalization and trade openness facilitating availability. On the supply-side, returns to scale afforded by new developing country markets can be exploited by large food manufacturers and multinationals, enabling even cheaper production of processed food already benefiting from lowered cost of production as a result of technological change.
Other Factors
A strong association between obesity rates and income disparities, which has been observed based on geographical comparison, may well hold across time considering that inequalities have been increasing in several countries over the years. Increase in female labor participation has been also proposed as a potential explanation for the decline in dietary quality and the consequent weight increase, especially for the younger generations. However, the link is not as clear as for technological change. Although there are studies showing that such an effect exists, it only explains a small portion of the observed growth in weight. Rapid urbanization is a further factor that has been associated with increasing obesity rates in developed countries mainly because life is thought to be more sedentary in cities, although it is difficult to define the causal direction of this relationship. Other economics-related explanations lie in the dramatic progress in medical treatment for obesity-related conditions, with a consequent decline in perceived risks which may work as a rational disincentive to conducting a healthy lifestyle.
Insufficient or biased (asymmetric) information (e.g., through advertising), often invoked as a driver for unhealthy behaviors at the individual level, is an unlikely determinant at the aggregate level, unless one assumes that the quality of nutrition and health information has worsened over the last two decades, despite most obesity policies having been targeted at public communication. The same argument holds for the role of education, an important explanatory factor for micro-level heterogeneity, but not particularly relevant (or even beneficial) when looking at the time series of obesity rates.
More recently, the focus of economists has turned to individual behavioral factors – especially behavioral failures – such as inconsistent time preference, addiction, and lack of self-control. As in the case of genetics or other biological factors, it is quite difficult to bring conclusive evidence on the role played by these individual-level factors. To do so, one has to once more accept that behavior at the population level (or its distribution) has rapidly changed over time, for which there is insufficient evidence, given available data.
Effects
Unhealthy diets in combination with lower physical activity levels and obesity have been linked to a range of noncommunicable diseases (NCDs), including several types of cancer, coronary heart disease, stroke, type II diabetes, osteoporosis, and osteoarthritis. There are a number of pathways from diets and physical activity to these diseases. Primarily through calorie balance (although there is some evidence that diet quality matters too), there is an impact on overweight and obesity, which are directly linked to many of these diseases. Overweight and obesity may also operate through intermediary conditions, such as hypertension and dyslipidemia to raise the risk of contracting some of these diseases. In addition, diets and physical activity may directly (rather than operating through an effect on risk of obesity) affect NCD risk, or through intermediary conditions as noted above. These effects impose a range of costs on the macroeconomy, classified as direct (medical) and indirect (productivity), as described below. Available estimates are largely for developed countries (see, e.g., http://www.youtube.com/watchv=mfnw ZrLKfoo), and there is a significant paucity of developing country cost estimates.
Direct Costs
The bulk of cost estimates relating to unhealthy diets and obesity relates to direct costs arising from increased medical expenditure on diagnosis, treatment, and management. A range of methods have been used in estimating these, ranging from cohort studies, where medical costs arising among groups of subjects varying by body mass index (BMI) ranges are examined over several years, to regression models, to studies based on dynamic simulation models of the relationship between BMI and NCD risks. These studies frequently extrapolate from study samples to the national population. Costs accruing to the national economy have been found to be substantial, as can be seen from Table 1, although it is worth noting the comparability across studies is complicated by differing protocols, methods and pathways and components taken into account (e.g., consideration of costs arising from obesity alone vs. costs arising from diet quality as well as obesity). A key issue in cost estimation relates to ‘lifetime costs’ – whether medical cost savings due to early mortality caused by obesity offsets the increased medical costs accrued during the lifetime of overweight and obese individuals. The limited research available on this issue is inconclusive, and this remains an area for future research.
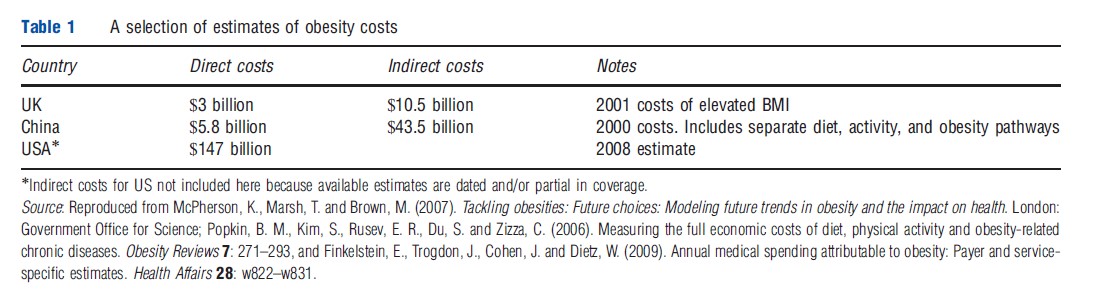
Indirect Costs
Indirect costs of obesity estimated in the literature encompass a range of nonmedical costs relating to productivity loss. These include absenteeism, disability, premature mortality, and presenteeism. Absenteeism and disability costs arise from time taken out of work due to obesity-related conditions. Premature mortality costs arise when workers die before retirement age due to obesity-related disorders. Presenteeism captures lowered efficiency at work arising from obesity-related disorders. There is debate about the extent to which lost time at work equates to lost productivity, because harder work from those present at work may compensate for time–input loss arising from obesity. As in the case of direct costs, available studies differ in terms of what they cover under indirect costs, and there are numerous measurement problems, prominent among these being distinguishing correlation from causation in measuring the effect of obesity on indirect costs. Table 1 shows that indirect costs can be very substantial, and can exceed direct costs by a significant margin in some countries.
Available estimates of the total burden of overweight and obesity, including direct as well as indirect costs, range from 0.2% to 0.6% of GDP in the developed west. For China, the estimate is as high as 4% of GDP.
Contemplating Hypothetical Scenarios: What Would The Implications Of Improved Diets Be?
The flip side of the earlier discussion on how changes in food consumption patterns have contributed to unhealthy dietary outcomes and NCDs, are the questions: (1) what would the larger sectoral/economy-wide implications of improved diets be and (2) what policies are needed to get there?
A sparse literature exists that estimates (simulates) the implications of moving toward recommended dietary norms, such as the World Health Organization (WHO) guidelines, at the population level. These show that the biggest negative consumption impacts would be on the animal products (meat, animal fats, and dairy products), vegetable oil, and feed cereal sectors. In Organization for Economic Cooperation and Development (OECD) countries, for example, consumption of animal products would shrink by between 15% and 30%, if WHO norms are to be met. However, the largest global effects would be generated by lowering meat consumption in rapidly growing economies such as China rather than in OECD countries.
Health benefits from such adherence to norms are likely to be substantially higher in developed and transitioning countries, where overnutrition is a more pressing concern, than in developing countries. However, patterns of international trade in agricultural products and general equilibrium effects imply that the effects of consumption changes in any large country or sets of countries are likely to be felt in other parts of the world, particularly developing countries. For example, a significant reduction in meat consumption in major markets, such as the EU, US, Canada, and Japan would have a substantial effect, notably a sharp increase in short-run unemployment in a large meat-exporting country such as Brazil. There is little evidence available to indicate that a global movement toward healthier diets can do much to enhance food and nutrition security in developing areas. The key implications of such movements are for meat consumption and for cereals used as feed. Although meat-exporting developing countries may suffer from reduced export opportunities, wheat and rice, the main staples used in developing countries have been shown to be little affected by such changes. However, it must be noted that the potential supply response from developing countries of a movement toward increased fruit and vegetable consumption is an area that has not been investigated thoroughly.
Policy For Better Diets
If overweight and obesity are accepted to be the outcome of individual utility maximizing decisions, then the economic rationale for public policy intervention has to be market failure. Foremost among these is externalities; people who choose to be overweight do not bear the full social cost of their actions, they are partially borne by others to the extent that health care is subsidized and employment law guarantees wages are paid when obesity-related ill health forces time off work. A second market failure occurs if information is imperfect, perfect information being a precondition for the informed choice underpinning utility maximization. Finally, food markets may display imperfect competition, specifically resulting in competition centered around advertising; food is an advertising-intensive industry, particularly fast food, confectionary, savory snacks, and soft drinks, largely viewed as principal culprits of the growth in obesity, particularly in the developed world.
In reality, governments also justify intervention for noneconomic reasons, notable among these being the correction of health inequalities (the socially deprived show a higher prevalence of obesity). Acting to change social norms has been used as a further justification for action; essentially this means changing people’s utility functions so that they choose to weigh less, comparison being made with the successes in changing attitudes to drunk-driving, smoking in public places, and wearing seat belts when driving. Children are often seen as a special case for whom more overt intervention to control is justified. More recently, behavioral economists have focussed attention on widespread systematic divergence from the rational behavior assumed by neoclassical economic models, arguing that such ‘behavioral failures’ have been exploited by the food industry to encourage higher consumption of processed foods; benevolent paternalism, it is argued can similarly exploit such behavioral failures to nudge people toward choosing healthier lifestyles they themselves would prefer (helping them to maximize their individual utilities).
The policy responses can be usefully grouped into two main categories, those actions centered around information and those which more directly intervene in markets. The actions which have been taken are shown in Table 2.
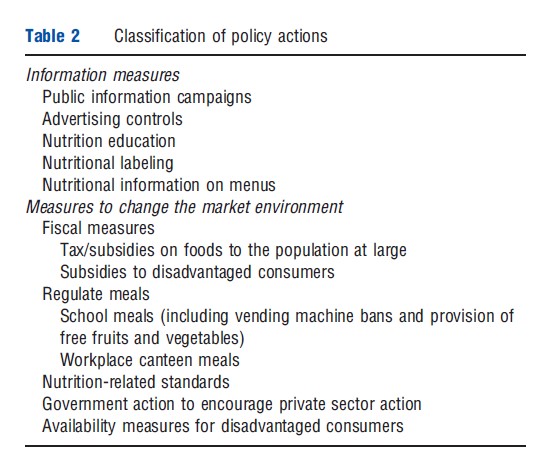
Of the information actions, public information campaigns exploit media communication and other social marketing tools to improve individual and social knowledge about health issues connected to food habits, and may be directed at any kind of target population. It is by far the most common healthy eating policy, together with education interventions. The aims may be simply to better inform people (e.g., about the health risks of obesity), or to change social norms. Advertising controls (bans) could in principle be used to limit advertising to adults and children if it was believed that all ages were encouraged to overeat by commercial advertising, though in practice, the measures have only been applied to children, presumably because it would be considered overly paternalistic to take such measures for adults. Nutrition education actions could likewise be used for adults or children, but have in practice only been used for children in schools. Nutrition labeling is essential to informed choices because the nutritional composition, notably number of calories, in foods, particularly processed foods, cannot be easily assessed, even by food scientists. Some form of labeling of the nutritional content of processed foods is compulsory in many developed countries and common even when not compulsory; the debate now is over the most effective form of communication using simplified messages, such as traffic lights to represent high, medium, or low levels of the major nutrients. There is a move toward extending labeling to food eaten outside the home in restaurant chains selling standardized products such as hamburgers.
Market intervention measures are less common. Fiscal measures have been proposed and widely assessed (simulated) by economists. On the positive side, taxes on unhealthy foods could be used to make people pay the full social cost of the food they eat, including the health care and economic productivity loss costs. Subsidies for healthy foods such as fruits and vegetables could be similarly justified as aligning social and private costs. The counterargument is that taxes would be regressive (the poor spend a higher share of their incomes on food), though there is some debate as to whether a fiscally neutral system where the subsidy cost exactly matches the tax revenue would suffer in this way. In any case, the measure would be highly unpopular with the food industry, and governments have not gone down this route, though small taxes, especially on soda, are widespread in the United States. One fiscal measure that has been employed, albeit to a limited extent, is subsidies, in the form of vouchers, to low-income households for the purchase of specific healthy foods. This is a promising area as it also addresses the issue of health inequalities, but may be deemed too expensive to apply in anything other than a very limited manner.
The other measures are all designed to influence the availability of foods, or rather nutrients. These tend to be targeted at diet quality more often than obesity per se, particularly measures to encourage food reformulation to reduce levels of salt, saturated fat, and trans fat in processed food; and measures to promote convenience stores in low-income areas to carry fruits and vegetables (the premise being that people in these areas without cars cannot access healthy food). The school food environment is commonly regulated to control the availability of junk foods (in canteens or vending machines) and the menus of meals (less chips, sausages, chicken nuggets, and hamburgers; and more salad, fruits, and vegetables). Menu control in public sector workplaces has been considered, but not widely applied.
References:
- Hawkes, C. (2006). Uneven dietary development: Linking the policies and processes of globalization with the nutrition transition, obesity and diet-related chronic diseases. Globalization and Health 2, 4.
- Lakdawalla, D., Philipson, T. and Bhattacharya, J. (2005). Welfare-enhancing technological change and the growth of obesity. American Economic Review 95, 253–257.
- Lock, K., Smith, R. D., Dangour, A. D., et al. (2010). Health, agricultural, and economic effects of adoption of healthy diet recommendations. Lancet. doi:10.1016/S0140-6736(10)61352-9.
- Mazzocchi, M., Traill, W. B. and Shogren, J. (2009). Fat economics: Nutrition, health and economic policy. Oxford: Oxford University Press.
- Msangi, S. and Rosegrant, M. (2011). Feeding the future’s changing diets: Implications for agriculture, markets, nutrition and policy. IFPRI 2020 conference paper. Washington: International Food Policy Research Institute.
- Popkin, B. M. (2003). The nutrition transition in the developing world. Development Policy Review 21, 581–597.
- Popkin, B. M., Kim, S., Rusev, E. R., Du, S. and Zizza, C. (2006). Measuring the full economic costs of diet, physical activity and obesity-related chronic diseases. Obesity Reviews 7, 271–293.
- Rosin, O. (2008). The economic causes of obesity: A survey. Journal of Economic Surveys 22, 617–647.
- Srinivasan, C. S., Irz, X. T. and Shankar, B. (2005). An assessment of the potential consumption impacts of WHO dietary norms in OECD countries. Food Policy 31, 53–77.
- Trogdon, J. G., Finkelstein, E. A., Hylands, T., Dellea, P. S. and Kamal-Bahl, S. J. (2008). Indirect costs of obesity: A review of the current literature. Obesity Reviews 9(5), 489–500.