The field of public mental health has made many advances, particularly since 1980. These developments include an increased understanding of the brain’s function through the study of neuroscience, the development of effective new medications and therapies, and the standardization of diagnostic codes for mental illnesses. However, many questions about mental health remain unanswered, and many people around the world are unable to benefit from the knowledge and treatments that are available.
Seven in ten Americans with a mental illness do not receive treatment. Biases against mental illness and lack of public awareness are among the obstacles that limit access to treatment and affect willingness to seek care. Fewer individuals with major psychiatric illnesses were institutionalized in the United States in the year 2000 than in 1980, but limited community resources had not yet met existing treatment needs. Over one-third of the homeless in the United States have a severe mental illness. The prevalence of dementia is rising as people are living longer, adding to the need for more resources. One of the main challenges for the field of mental health is overcoming the gap between an increasingly sophisticated understanding and treatment of mental illness and the availability of these advances to individuals and populations in need.
Mental, or psychiatric, illnesses are a major public health concern. They adversely affect functioning, economic productivity, the capacity for healthy relationships and families, physical health, and the overall quality of life. They cut across racial, ethnic, and socioeconomic lines to affect a significant proportion of communities worldwide. They tend to develop and manifest in the early adult years, often preventing individuals from leading full and productive lives. The National Comorbidity Survey of 1994 found nearly half of the individuals in its random U.S. sample had a psychiatric disorder over their lifetime, and almost 30 percent had one in the past year. The World Health Organization’s World Health Report 1998 lists mood and anxiety disorders among the leading causes of morbidity and mood disorders as the leading cause of severely limited activity. Mental disorders account for a quarter of the world’s disability. Comorbidity (having more than one illness) is common and even further increases the risk of disability. Suicide is the eighth leading cause of death in the United States and the third leading cause in the fifteen- to twenty-four-year-old age group. More people die by suicide than homicide.
Dianne Hales and Robert Hales define mental health as
the capacity to think rationally and logically, and to cope with the transitions, stresses, traumas, and losses that occur in all lives, in ways that allow emotional stability and growth. In general, mentally healthy individuals value themselves, perceive reality as it is, accept its limitations and possibilities, respond to its challenges, carry out their responsibilities, establish and maintain close relationships, deal reasonably with others, pursue work that suits their talent and training, and feel a sense of fulfillment that makes the efforts of daily living worthwhile (p. 34).
A healthy pregnancy, adequate parenting, secure attachments to caretakers, regular involvement in groups, and stable intimate relationships all contribute to the development and maintenance of mental health. Mental health does not imply the absence of distress and suffering, or strict societal conformity. Mental health and illness, idiosyncratic beliefs and delusions, sadness and depression, and worry and severe anxiety lie on a continuum. An essential criterion for defining behavioral patterns or symptoms of psychological distress as a mental disorder is that they become significant enough to be functionally disabling and impose substantial increased risks ranging from an important loss of freedom to suffering pain, disability, or death.
Both genetic inheritance and environmental factors influence one’s vulnerability to mental illness. Twin and family studies and genetic research have demonstrated the former, though specific genes have been difficult to identify, and there may be multiple genes involved in most psychiatric disorders. Traumatic events throughout one’s lifetime, including childhood abuse or neglect, major losses, violence, military combat, and dislocation (as among the urban homeless or wartime refugees) are known to threaten mental stability. Nontraumatic stressors, including unemployment, bereavement, and relational or occupational problems, can impact mental health. Nutritional deficiencies (such as vitamin B12), infections (such as syphilis and HIV [human immunodeficiency virus]), and heavy metal poisoning (such as lead) can all cause psychiatric syndromes. Substance abuse contributes significantly to the exacerbation or even precipitation of other psychiatric illnesses and complicates their treatment. Poverty and homelessness are risk factors for many of these problems, but may also be the outcome of psychiatric illness and the inability to function independently.
Many models of mental health and illness have been proposed. Emil Kraepelin (1856–1926) contributed to the development of the precise categorization of mental illnesses, particularly in distinguishing the long-term course of psychotic and mood disorders. Sigmund Freud (1856–1939) developed the theory of psychoanalysis, through which he claimed that symptoms of psychiatric disorders, as well as many phenomena of everyday life, have unconscious meanings and sources. Erik Erikson (1902–1994) formulated a theory of human development with specific tasks and crises at different stages of the life cycle. Failure to master these stages can lead to various forms of psychopathology. Neuroscientists have demonstrated molecular models of illness, which involve genetic, developmental, functional, anatomical, and molecular abnormalities of the brain. The biopsychosocial model, proposed by George Engel in the 1970s, integrates the biological, genetic, and molecular mechanisms of illness with a psychological understanding of personality development and response to stress as well as social, cultural, and environmental influences.
The Diagnostic and Statistical Manual of Mental Disorders (its 4th edition, DSM-IV, was published in 1994) is the product of research on standardized diagnostic criteria aimed at creating a common, validated descriptive system for all mental health care providers. It is nearly universally accepted, as it classifies and describes categories of illness and aims to be neutral about controversial theories of etiology (see Table 1). The following descriptions of various mental disorders are based on DSM-IV criteria.
Table 1. Lifetime and 12-month prevalence of DSM-III-R disorders
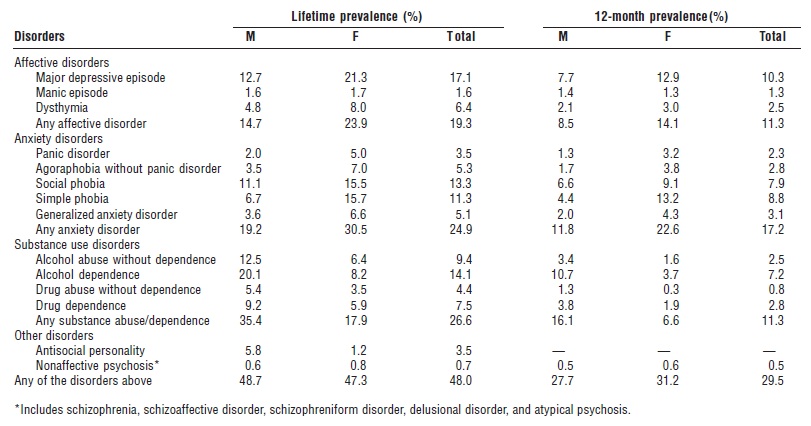
SOURCE: Kessler, R.C. et al. (1994). “Lifetime and Twelve–Month Prevalence of DSM–III–R Psychiatric Disorders in the United States: Results from the National Comorbidity Study.” Archives of General Psychiatry 51:8–19.
Affective disorders involve a cyclical pattern of significant mood disturbance. A major depressive episode may be precipitated by a stressful life situation but also has genetic factors. Disturbances in appetite, sleep, energy, concentration, and sexual interest are common symptoms. The majority of patients respond to treatment with antidepressant medication and/or psychotherapy. An individual who has long-term (over two years) of minor to moderate depressive symptoms may have dysthymia. Substance abuse, medical disorders (such as hypothyroidism), and normal life cycle events in which hormonal changes are prominent (such as the postpartum period) can all cause symptoms of depression and should be considered carefully during an assessment. An adjustment disorder is a milder disturbance of mood that may occur in response to a stressful life situation, such as a personal loss or financial crisis, and that usually resolves when the stress is relieved. About 1 percent of the general population has bipolar disorder, also called manic-depressive disorder, in which manic episodes are present as well as depressive episodes. Mania is characterized by a persistently elevated or irritable mood for at least a week, often with decreased need for sleep, rapid speech, impulsivity in spending and other behaviors, and grandiosity. In more severe manic and depressive episodes, psychotic symptoms may emerge, which can complicate treatment. Bipolar disorder is treated with mood stabilizers, such as lithium or valproic acid, and supportive management. Antidepressant medications alone can precipitate mania in susceptible patients.
Psychotic disorders are characterized by “positive” symptoms such as hallucinations, delusions, and bizarre behaviors, as well as “negative” symptoms such as paucity of speech, poverty of ideas, blunting of affective expression, and functional deterioration. Cognitive problems such as disorganization of thought processes also occur. Schizophrenia is a chronic, disabling illness that affects almost 1 percent of the world population, independent of ethnic or cultural background. Risk factors include a family history and possibly psychosocial stressors. The precise cause is still unknown, but it is clear that certain areas of the brain and certain neurotransmitters are involved. Many of those affected are unable to maintain work or relationships and require supportive services to help them manage basic needs such as shelter and food. Treatment includes antipsychotic medication, comprehensive social services including social and occupational rehabilitation if possible, and substance abuse treatment if necessary. Newer antipsychotic medications such as clozapine, olanzapine, and risperidone have been able to treat more symptoms generally with fewer side effects, allowing many to lead more productive lives. Some patients with schizophrenic-type illness also experience prominent affective symptoms nonconcurrently and may have schizoaffective disorder. These patients often require a mood stabilizer as well as antipsychotic medication. Substance use, especially hallucinogens and stimulants (such as amphetamines and cocaine), can precipitate psychotic symptoms, and these may even endure beyond the period of substance use. Some medical conditions (such as epilepsy and delirium) and some medications (such as steroids) can also cause psychotic symptoms and should be considered in the assessment and treatment of psychosis.
Anxiety disorders are among the most prevalent psychiatric disorders in the general population, and these disorders lead to both psychological distress and increased health care utilization. Panic disorder often manifests with somatic symptoms, such as palpitations, chest pain, nausea, trembling, dizziness, and shortness of breath, and can be easily confused with a medical disorder by both patients and doctors. Patients develop persistent concerns about having further panic attacks. Some develop agoraphobia, or a fear of being in public places where their attacks may be triggered. Other phobias include simple phobia, such as fear of heights or specific animals, and social phobia, which is a marked and persistent fear of certain or all social situations, such as speaking in public or being around others in general. People with obsessive-compulsive disorder have obsessions, characterized by recurrent or persistent thoughts, impulses, or images that are experienced as intrusive and inappropriate, and/or compulsions, characterized by repetitive behaviors or mental acts often performed in response to an obsession. After one experiences a traumatic event, in which actual or threatened death or severe injury is witnessed or experienced, one may develop post-traumatic stress disorder. Intrusive recollections of the event (such as nightmares), avoidance of reminders of the event, and increased arousal (such as increased vigilance for potential threats) can all cause significant distress and impairment following a wide range of traumatic events, including an accident, military combat, torture, or rape. Generalized anxiety disorder is characterized by excessive and persistent anxiety or worry about a number of events or activities, such as work or school performance. For all anxiety disorders, specific psychopharmacologic and psychotherapeutic (such as cognitive-behavioral therapy) techniques of treatment can be effective and complementary.
Substance-use disorders are quite common and occur in all segments of society. They can lead to accidents, violent crime, and major problems in school and at work. They can cause or complicate various medical and psychiatric illnesses. Liver failure, ulcers, heart attacks, cognitive disorders, and depression are among the potential outcomes of various substances. These disorders pose major public health concerns for public safety, health costs, economic productivity, and pregnancy risks, among others. Substance abuse is defined as a maladaptive pattern of use indicated by continued use despite persistent or recurrent social, occupational, psychological, or physical problems caused or exacerbated by the use of the substance; or recurrent use in situations that could be physically hazardous (such as driving while intoxicated). With substance dependence, signs of physical dependence such as withdrawal symptoms are often present, and the person spends a great deal of time involved in substance-related activities, uses more of the substance than intended, is unable to cut down, and continues to use the substance despite social, occupational, or physical problems related to it. The first steps of treatment involve developing insight, acknowledging the problem, and wanting to change. There are various self-help groups (such as Alcoholics Anonymous), comprehensive treatment programs, psychosocial interventions, and medications that can help lead to successful recovery for the majority of those with substance use disorders.
Childhood disorders include pervasive developmental disorders, such as autism, which occurs in four out of ten thousand people; mental retardation, which can be caused by a variety of genetic abnormalities or prenatal insults; and attention deficit–hyperactivity disorder, which can lead to significant problems in school and in social relationships. Childhood abuse and neglect are tragically quite common, with one million children affected annually in the United States alone. These can have major adverse effects on development of personality, relationships, and the ability to function in the world.
Personality disorders are usually first evident in late adolescence and are characterized by pervasive, persistent maladaptive patterns of behavior that are deeply ingrained and are not attributable to other psychiatric disorders. Biological and genetic factors, as well as developmental difficulties, are significant contributors. Other disorders described in DSM-IV include eating disorders, with restriction (anorexia) and/or binging and purging (bulimia) and impulse control disorders (e.g., kleptomania). Somatoform disorders cause physical symptoms with no apparent medical cause (e.g., hysterical paralysis).
Gender, race, ethnicity, and culture are important factors in determining the expression and risk of mental disorders, and these factors also impact on treatment considerations. Certain disorders are more prevalent in women, such as depression and eating disorders, and some in men, such as substance abuse. Cultural background may influence the idioms of psychological distress. For example, nervios describes for many Latinos a constellation of somatic, anxiety, and depressive symptoms distinct from particular DSM-IV diagnoses. Psychiatric disorders are the main risk factor for suicide, but rates vary significantly depending on gender, age, race, religion, marital status, and culture.
Bibliography:
- Bromet, E. J. (1998). “Psychiatric Disorders.” In Maxcy- Rosenau-Last Public Health and Preventive Medicine, 14th edition, ed. Robert B. Wallace. Stamford, CT: Appleton and Lange.
- Diagnostic and Statistical Manual of Mental Disorders (DSMIV) (1994), 4th edition. Washington, DC: American Psychiatric Association.
- Eisendrath, S. J., and Lichtmacher, J. (1999). “Psychiatric Disorders.” In Current Medical Diagnosis and Treatment 1999, eds. L. M. Tierney, Jr., S. J. McPhee, and M. A. Papadakis. Stamford, CT: Appleton and Lange.
- Engel, G. (1980). “The Clinical Application of the Biopsychosocial Model.” American Journal of Psychiatry 137(5):535–544.
- Hales, D., and Hales, R. E. (1995). Caring for the Mind: The Comprehensive Guide to Mental Health. New York: Bantam Books.
- Jamison, K. R. (1999). Night Falls Fast. New York: Alfred Knopf.
- Kaplan, Harold I., and Sadock, Benjamin J., eds. (1995). Comprehensive Textbook of Psychiatry. 6th edition. Philadelphia: Williams and Wilkins.
- Kessler, R. C.; McGonagle, K. A.; Zhao, S.; Nelson, C. B.; Hughes, M.; Eshleman, S.; Wittchen, H. U.; and Kendler, K. S. (1994). “Lifetime and Twelve Month Prevalence of DSM-III-R Psychiatric Disorders in the United States: Results from the National Comorbidity Study.” Archives of General Psychiatry 51:8–19.
- S. Public Health Service (1999). The Surgeon General’s Call to Action to Prevent Suicide. Washington, DC: Author.
- World Health Organization (1998). World Health Report 1998: Life in the Twenty-first Century, A Vision for All. Report of the Director-General. Geneva: Author.