Introduction
Despite great improvements in the oral health of populations in several countries, global problems still persist. This is particularly so among the underprivileged groups in both developing and developed countries. Oral disease conditions such as dental caries, periodontal disease, tooth loss, oral cavity cancers, HIV/AIDS-related oral disease, and oro-dental trauma are major public health problems worldwide. Poor oral health may have a profound effect on general health. The experience of pain, and problems with eating, chewing, smiling, and communication due to missing, discolored, or damaged teeth have a major impact on people’s daily lives and well-being. Furthermore, oral diseases restrict activities in school, at work, and at home causing millions of school and work hours to be lost each year the world over.
The objectives of the present article are to outline the oral disease burden globally and to highlight the influence of major sociobehavioral risk factors related to oral health. Sources of information are the World Health Organization (WHO) Global Oral Health Data Bank (Petersen, 2003; WHO, 2004), including scientific reports from population studies carried out in various countries. For the majority of countries, WHO standardized criteria for clinical registration of oral disease conditions are that applied and calibration trials be conducted accordingly for the control of quality of data and assessment of interexaminer variability (WHO, 1997). The data stored in the data bank are updated regularly.
The Burden of Dental Disease
Dental caries (tooth decay) and periodontal disease (gum disease) have historically been considered the most important global oral health burdens. Dental caries is still a major health problem in most industrialized countries as the disease affects 60% to 90% of school-aged children and the vast majority of adults (Petersen, 2003; WHO, 2004). At present, the distribution and severity of dental caries vary in different parts of the world and within the same region or country. Figure 1 illustrates the dental caries experience levels (severity) in permanent teeth as measured in 12-year-olds by the Decayed, Missing and Filled Teeth index (DMFT). The disease level in children is relatively high in the Americas (DMFT?3.0) and in the European Region (DMFT?2.6), whereas it is less common or less severe in the African region (DMFT?1.7) (Petersen, 2003;WHO, 2004). Figure 2 illustrates the time trends in dental caries experience of 12-year-old children in developing and developed countries. In most developing countries, dental caries levels were low until recent years. Now, however, dental caries prevalence rates and dental caries experience tend to increase. This is due particularly to the growing consumption of sugars and to inadequate exposures to fluorides. In contrast, a caries decline has been observed in most industrialized countries over the past 20 years or so. This pattern was the result of a number of public health measures, including effective use of fluorides, coupled with changing living conditions, healthier lifestyles, and improved self-care practices.
Figure 1
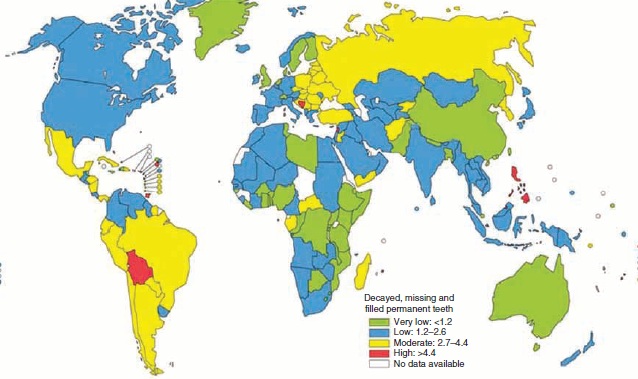
Dental caries levels (DMFT) of 12-year-olds worldwide. Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of theWHOGlobal Oral Health Programme. Community Dentistry and Oral Epidemiology 31(Suppl 1): 3–24; WHO (2004) Global Oral Health Data Bank. Geneva, Switzerland: WHO.
Figure 2
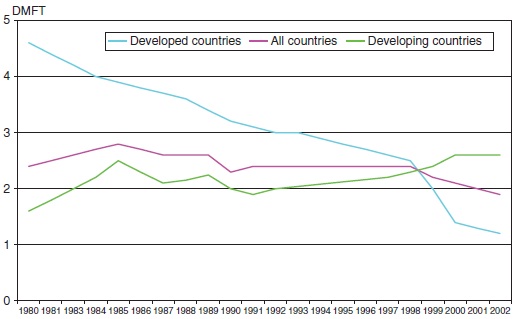
Changing levels of dental caries experience (DMFT) among 12-year-olds in developed and developing countries. Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 31(Suppl 1): 3–24; WHO (2004) Global Oral Health Data Bank. Geneva, Switzerland: WHO.
Worldwide, dental caries prevalence is high among adults as the disease affects nearly 100% of the population in the majority of countries. Figure 3 outlines the dental caries levels among 35- to 44-year-olds, as measured by the mean DMFT index (Petersen, 2003; WHO, 2004). Most industrialized countries and some countries of Latin America show high-DMFT values (i.e., 14 teeth or more), while dental caries experience levels are much lower in the developing countries of Africa and Asia. In several industrialized countries older people often have had their teeth extracted early in life because of pain or discomfort, leading to reduced quality of life. The proportion of adults with no natural teeth (edentulous) aged 65 years or more is still high in some countries (Table 1); meanwhile, in many industrialized countries there has been a positive trend of reduction in tooth loss among older adults in recent years (Chen et al., 1997) (Figure 4), in parallel with increased seeking of preventive oral care services (Petersen et al., 2004).
Figure 3
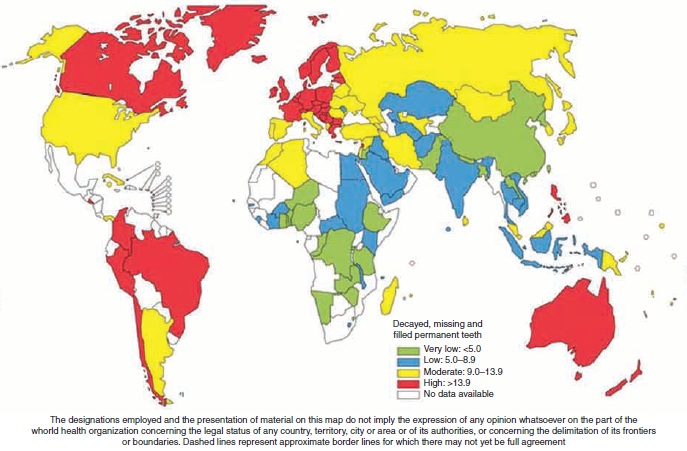
Dental caries levels (DMFT) of 35- to 44-year-olds worldwide. Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 31(Suppl 1): 3–24; WHO (2004) Global Oral Health Data Bank. Geneva, Switzerland: WHO.
Table 1 Prevalence of edentulousness (%) of elderly reported for selected countries throughout the world
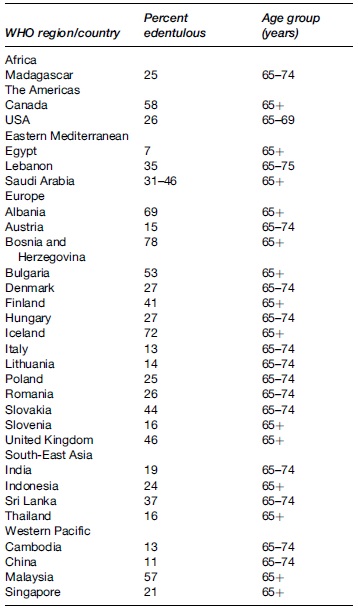
Reproduced from Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 31 (Supplement 1): 3–24; and WHO (2004) Global Oral Health Data Bank. Geneva: WHO.
Figure 4
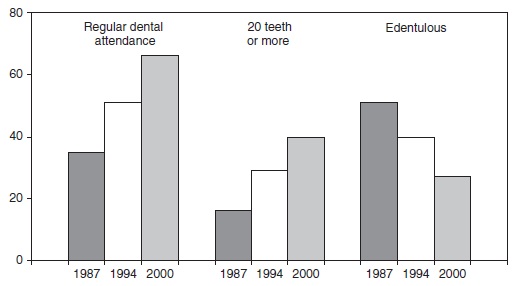
Percentages of 65- to 74-year-olds in Denmark who have regular (annual) dental attending habits, functional dentition (20 teeth or more), and without natural teeth (edentulous), by year of observation. Petersen PE, Kjoller M, Christensen LB, and Krustrup U (2004) Changing dentate status of adults, use of dental health services, and achievement of national dental health goals in Denmark by the year 2000. Journal of Public Health Dentistry 64: 127–135.
In developing countries, oral health services are mostly offered from regional or central hospitals in urban centers, and little if any importance is given to preventive or restorative dental care. Many countries of Africa, Asia, and Latin America have a shortage of oral health personnel and generally the capacity of the systems is limited to pain relief or emergency care. In Africa, the dentist to population ratio is approximately 1:150 000, against about 1:2000 in most industrialized countries. In children and adults suffering from severe tooth decay, teeth are often left untreated or are extracted to relieve pain or discomfort. In the future, tooth loss and impaired oral function are therefore expected to increase as a public health problem in many developing countries.
Tooth loss in adult life may also be attributable to poor periodontal health. Severe periodontitis, which may result in tooth loss, is found in 5% to 20% of most adult populations worldwide. Figure 5 illustrates the prevalence of symptoms of disease among 35- to 44-year-olds by WHO region (Petersen, 2003; WHO, 2004; Petersen and Ogawa, 2005), using the so-called Community Periodontal Index (Score 0 = individuals with healthy periodontal conditions; Score 1 = individuals with bleeding from gums; Score 2 = individuals with bleeding gums and calculus; Score 3 = individuals with shallow periodontal pockets (4–5mm); Score 4 = individuals with deep periodontal pockets (6mmor more)). Symptoms of periodontal disease are highly prevalent among adults within all regions; furthermore, from a global perspective, most children and adolescents have signs of gingivitis (gum disease) (WHO, 2004). Aggressive periodontitis, a severe periodontal condition affecting individuals during puberty and that may lead to premature tooth loss, affects about 2% of youth (Albander, 1997).
Figure 5
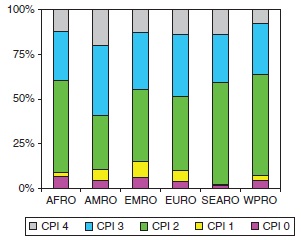
Mean percentages of maximum Community Periodontal Index (CPI) scores in 35- to 44-year-olds by WHO Regional Offices. Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 31(Suppl 1): 3–24; WHO (2004) Global Oral Health Data Bank. Geneva, Switzerland: WHO; Petersen PE and Ogawa H (2005) Strengthening the prevention of periodontal disease: The WHO approach. Journal of Periodontology 76: 2187–2193.
Oral Cancer
Oral cavity cancer is more common in developing than developed countries (Figure 6 and Figure 7) (Stewar t and Kleihues, 2003; WHO, 2004).The prevalence of oral cavity cancer is particularly high among men, the eighth most common cancer worldwide. In South-Central Asia, cancer of the oral cavity ranks among the three most common types of cancer. In India, the age-standardized incidence rate of oral cancer is 12.6 per 100 000 population. It is noteworthy that sharp increases in the incidence rates of oral cancers have been reported for several countries and regions such as Denmark, France, Germany, Scotland, and Central and Eastern Europe, and, to a lesser extent, Australia, Japan, New Zealand, and the United States (Stewart and Kleihues, 2003; WHO, 2004), due to high consumption of tobacco and alcohol.
Figure 6
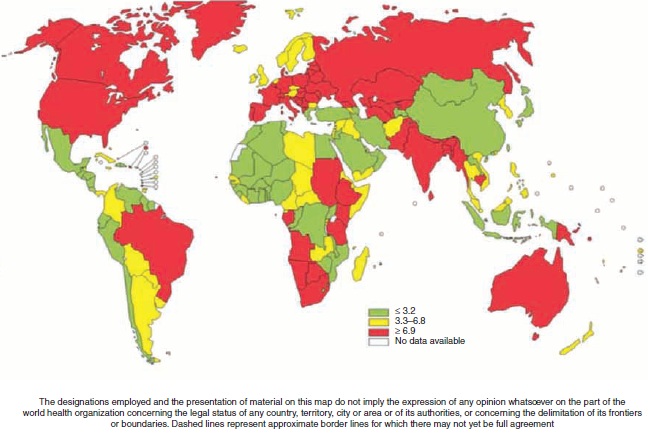
Incidence of oral cavity cancer among males (age-standardized rate (ASR) per100 000 world population). Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 31(Suppl 1): 3–24; WHO (2004) Global Oral Health Data Bank. Geneva, Switzerland: WHO.
Figure 7
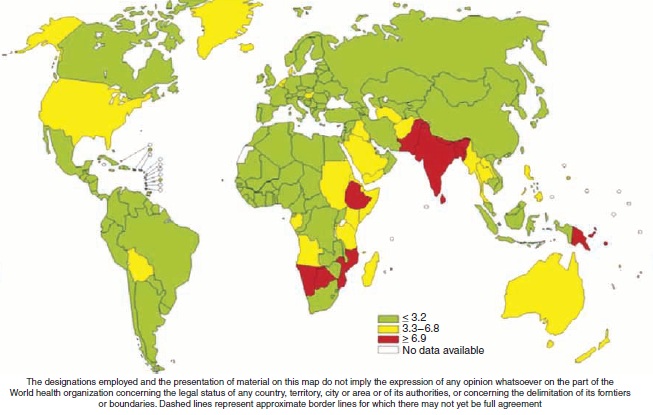
Incidence of oral cavity cancer among females (age-standardized rate (ASR) per 100 000 world population). Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 31(Suppl 1): 3–24; WHO (2004) Global Oral Health Data Bank. Geneva, Switzerland: WHO.
Oral Health in HIV/AIDS
A number of studies have demonstrated the negative impact on oral health of HIV infection (Coogan et al., 2005). Approximately 40% to 50%ofHIV-positive persons have oral fungal, bacterial, or viral infections often occurring early in the course of the disease. Oral lesions strongly associated with HIV infection are pseudo-membranous oral candidiasis, oral hairy leukoplakia, HIV gingivitis and periodontitis, Kaposi sarcoma, and non-Hodgkin’s lymphoma. Dry mouth as a result of decreased salivary flow rate may not only increase the risk of dental caries but negatively impact quality of life because of difficulty in chewing, swallowing, and tasting food. The need for oral health care in terms of immediate care and referral, treatment of manifest oral disease, prevention, and health promotion is particularly high among the under-served, disadvantaged population groups of developing countries, including HIV-infected people (Coogan et al., 2005).
Noma – Cancrum Oris
Noma, a debilitating oro-facial gangrene, is an important disease burden in many developing countries, particularly in Africa and Asia (Figure 8) (Petersen, 2003). Noma primarily begins as a localized gingival ulceration and spreads rapidly through the oro-facial tissues, establishing itself with a blackened necrotic center (Enwonwu, 1995). About 70% to 90% of cases are fatal in the absence of care. Fresh noma is seen predominantly in the age group 1–4 years, although late stages of the disease occur in adolescents and adults. Poverty is the key risk condition for development of noma; the environment inducing noma is characterized by severe malnutrition and growth retardation, unsafe drinking water, deplorable sanitary practices, residential proximity to unkempt animals, and a high prevalence of infectious diseases such as measles, malaria, diarrhea, pneumonia, tuberculosis, and HIV/AIDS.
Figure 8
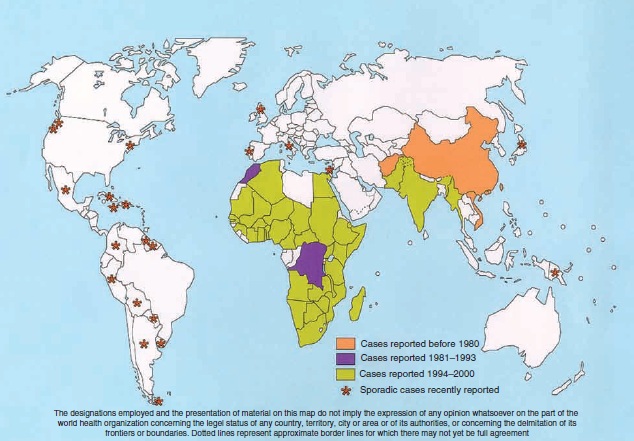
Cases of noma (cancrum oris) reported around the world. Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 31(Suppl 1): 3–24.
Oro-Dental Trauma
In contrast to dental caries and periodontal disease, reliable data on the frequency and severity of oro-dental trauma are still lacking in most countries, particularly in developing countries (Andreasen and Andreasen, 2002). Some countries in Latin America report dental trauma in about 15% of schoolchildren, while prevalence rates of 5% to 12% are found in children aged 6 to 12 years in the Middle East. Furthermore, studies from certain industrialized countries have revealed that the prevalence of dental traumatic injuries is on the increase, ranging from 16% to 40% among 6-year-old children and from 4% to 33% among 12- to 14-year-old children (Andreasen and Andreasen, 2002). A significant proportion of dental trauma relates to sports, unsafe playgrounds or schools, road accidents, and violence.
Dental Erosion
Dental erosion is the progressive, irreversible loss of dental hard tissue which is chemically etched away from the tooth surface by extrinsic and/or intrinsic acids. Dental erosion appears to be a growing problem in several countries, affecting 8% to 13% of adults (ten Cate and Imfeld, 1996), and increasing levels are thought to be due to higher consumption of acidic beverages (i.e., soft drinks, fruit juices). Worldwide, there is a need for more systematic population-based studies on the prevalence of dental erosion using a standard index of measurement.
Developmental Disorders
Congenital diseases of the enamel or dentine of teeth, problems related to the number, size, and shape of teeth, and craniofacial birth defects such as cleft lip and/or palate (CL/P) are most important. The incidence of CL/P varies tremendously worldwide. Native Americans in North America show the highest incidence rates at 3.74 per 1000 live births, whereas a fairly uniform incidence of 1:600 to 1:700 live births are reported among Europeans (WHO, 2002). The incidence rates appear high among Asians (0.82–4.04 per 1000 live births), intermediate in Caucasians (0.9–2.69 per 1000 live births), and low in Africans (0.18–1.67 per 1000 live births). The causes of CL/P are complex, involving multiple genetic and environmental risk factors. Risk factors such as folic acid deficiency, maternal smoking, and maternal age have particularly been implicated in the formation of clefts (WHO, 2002).
Malocclusion is not a disease but rather a set of dental deviations that in some cases can influence quality of life. Estimates of different traits of malocclusion are available from a number of countries, primarily in Northern Europe and North America. For example, prevalence rates of dento-facial anomalies in Northern Europe and North America are reported at about 10%, according to the Dental Aesthetic Index (Chen et al., 1997). Other conditions that may lead to special health-care needs include Down syndrome, cerebral palsy, learning and developmental disabilities, and genetic and hereditary disorders with oro-facial defects.
There is no consistent evidence of time trends in development disorders, nor is there consistent variation by socioeconomic status, but these aspects have not been adequately studied (WHO, 2002). In addition, there are many parts of the world in which there is little or no information available on the frequency of developmental disorders, in particular, parts of Africa, Central Asia, Latin America, the Middle East, and Eastern Europe.
Fluorosis of Teeth
Dental fluorosis develops during formation of teeth when children are young. Drinking water with more than 1.5 ppm (parts per million) of fluoride can give rise to enamel defects and discoloration of teeth leading to endemic fluorosis in the population. These may differ in intensity from mild to severe. For example, in East Africa, in the Great Rift Valley area, and in some parts of India and north Thailand, the groundwater has very high levels of fluoride. In such areas, dental fluorosis may be found in the majority of people (WHO, 1994). Fluorosis of teeth can also occur in individuals in developed countries due to widespread use of certain forms of fluorides for prevention of dental caries, although the degree of fluorosis is mostly very mild when compared with endemic fluorosis.
The Economic Impact of Oral Disease
Traditional treatment of oral disease is extremely costly, the fourth most expensive disease to treat in most industrialized countries. In industrialized countries, the burden of oral disease has been tackled through establishment of advanced oral health systems which primarily offer curative services to patients. Most systems are based on demand for care and oral health care is provided by private dental practitioners to patients, with or without third-party payment schemes. Some countries, including those of Scandinavia and the United Kingdom, have organized public health services, particularly providing oral health care to children and disadvantaged population groups. Traditional curative dental care is a significant economic burden on many industrialized countries where 5% to 10% of public health expenditure relates to oral health (U.S. Department of Health, 1998; Widstro?m and Eaton, 2004). Over the past years, savings in dental expenditures have been noted for industrialized countries which have invested in preventive oral care and where positive trends are observed in terms of reduction in the prevalence of oral disease.
In most developing countries, investment in oral health care is low. In these countries, resources are primarily allocated to emergency oral care and pain relief; if treatment were available, the costs of dental caries in children alone would exceed the total health-care budget for children (Petersen, 2003).
Oral Disease Burdens and Risk Factors
The current global and regional patterns of oral disease largely reflect distinct risk profiles across countries, related to living conditions, lifestyles, and the implementation of preventive oral health systems. The significant role of sociobehavioral and environmental factors in oral disease and health is shown in a large number of epidemiological surveys (Chen et al., 1997). Socioepidemiological studies have been carried out particularly in relation to dental diseases; for developed and increasingly for developing countries these studies observe that the burden of disease, poor quality of life, and the need for care are highest amongst the poor or disadvantaged population groups. The sociobehavioral risk factors in dental caries are found to play significant roles worldwide for both children and adults (Petersen, 2005). Some countries report tooth loss to be higher in women than in men as women more often seek dental care (Chen et al., 1997).
A core group of modifiable risk factors is common to many chronic diseases and injuries. The four most prominent noncommunicable diseases – cardiovascular diseases, diabetes, cancer, and chronic obstructive pulmonary diseases – share common risk factors with oral diseases, preventable risk factors that are related to lifestyles. For example, dietary habits are significant to the development of chronic diseases and influence the development of dental caries. Oral cavity bacteria are involved in progression of dental diseases such as dental caries and periodontal disease. Most important, excessive amounts and frequent consumption of sugars are major causes of dental caries and the risk of caries is high if population exposure to fluorides is inappropriate. In addition, tobacco use has been estimated to account for over 90% of cancers in the oral cavity, and is associated with aggravated periodontal breakdown, poorer standards of oral hygiene, and thus premature tooth loss (Petersen, 2003). The oral cancer risk increases when tobacco is used in combination with alcohol or areca nut. In Asia, incidence rates of oral cancer are high and relate directly to smoking, use of smokeless tobacco, and alcohol consumption.
The strong correlation between several oral diseases and noncommunicable chronic diseases is primarily a result of the common risk factors. Many general disease conditions also have oral manifestations that increase the risk of oral disease, which, in turn, is a risk factor for a number of general health conditions. Severe periodontal disease, for example, is associated with diabetes mellitus and has been considered the sixth complication of diabetes (Petersen and Ogawa, 2005).
Conclusion
Given the extent of the problem, oral diseases are major public health problems in all regions of the world. Their impact on individuals and communities as a result of pain and suffering, impairment of function, and reduced quality of life, is considerable. Globally, the greatest burden of oral diseases is on the disadvantaged and poor population groups. The current pattern of oral disease reflects distinct risk profiles across countries related to living conditions, lifestyles, and environmental factors, and the implementation of preventive oral health systems. Global strengthening of public health programs through implementation of integrated oral disease prevention measures and health promotion is urgently needed, and use of common risk factors approaches should incorporate oral health within national health programs.
Bibliography:
- Albander JM, Brown LJ, and Lo? e H (1997) Clinical features of early-onset periodontitis. Journal of the American Dental Association 128: 1393–1399.
- Andreasen JO and Andreasen FM (2002) Dental trauma. In: Pine C (ed.) Community Oral Health, pp. 94–99. London: Elsevier Science.
- Chen M, Andersen RM, Barmes DE, Leclerq M-H, and Lyttle SC (1997) Comparing Oral Health Systems: A Second International Collaborative Study. Geneva, Switzerland: WHO.
- Coogan M, Greenspan J, and Challacombe SJ (2005) Oral lesions in infection with human immunodeficiency virus. Bulletin of the World Health Organization 83: 700–706.
- Enwonwu CO (1995) Noma: A neglected scourge of children in sub- Saharan Africa. Bulletin of the World Health Organization 73: 541–545.
- Petersen PE (2003) The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – the approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 31(Suppl 1): 3–24.
- Petersen PE (2005) Sociobehavioural risk factors in dental caries: International perspectives. Community Dentistry and Oral Epidemiology 33: 274–279.
- Petersen PE, Kjo? ller M, Christensen LB, and Krustrup U (2004) Changing dentate status of adults, use of dental health services, and achievement of national dental health goals in Denmark by the year 2000. Journal of Public Health Dentistry 64: 127–135.
- Petersen PE and Ogawa H (2005) Strengthening the prevention of periodontal disease: The WHO approach. Journal of Periodontology 76: 2187–2193.
- Stewart BW and Kleihues P (2003) World Cancer Report. Lyon, France: WHO International Agency for Research on Cancer.
- ten Cate JM and Imfeld T (1996) Dental erosion, summary. European Journal of Oral Sciences 104: 241–244.
- S. Department of Health (1998) National Health Expenditures, 1998. Washington, DC: Health Care Financing Administration.
- WHO (1994) Fluorides and oral health. Technical Report Series No. 846. Geneva, Switzerland: WHO.
- WHO (1997) Oral Health Surveys: Basic Methods, 4th edn. Geneva, Switzerland: WHO.
- WHO (2002) Global Strategies to Reduce the Health Care Burden of Craniofacial Anomalies. Geneva, Switzerland: WHO.
- WHO (2004) Global Oral Health Data Bank. Geneva, Switzerland: WHO. Widstrom E and Eaton KA (2004) Oral health care systems in the extended European Union. Oral Health and Preventive Dentistry 2: 155–194.