Being efficient means ‘doing something well without wasting time or energy.’ To economists, efficiency is a relationship between ends and means. What is important to note is that economists refer to the relationship between the value of the ends and means, not physical quantities. In economic terms, the value of using resources is equivalent to the maximum value that the resources could have generated in alternative use, and is often referred to as the opportunity cost. The acknowledgment that all actions are associated with various degrees of opportunity costs is at the core of economics, the goal being to generate the maximum benefit with available resources. This goal requires two conditions to be fulfilled: (1) that benefits are generated at the lowest minimum cost, so that overall benefits can be maximized and (2) that the right goods or services are produced in order to generate the maximum benefits. Basically it is a question of what should be produced and how is it best produced.
How and what to produce are questions that are answered differently depending on perspective. The ‘how’ mainly relates to how the production of a given health care service is organized. A leader of a health care firm may want to minimize production costs to his/her firm, thus keeping focus on minimizing costs relating to his/her own part of the production line, without keeping an eye on overall societal costs. Cost shifting may take place, and an efficient production of health care services from a hospital manager’s perspective may not necessarily mean that the production is efficient from the perspective of society as a whole. The ‘what’ should be produced is also a matter of perspective. Which services generate the most benefit can be defined in terms of a consumer’s or patient’s willingness to pay (WTP) for the health care service. Alternatively, it can be defined in terms of health gains or other goals that are thought to be beneficial to the recipients of health care services or society. When reading health economic analyses that seek to portray efficiency issues, one should be wary of which budgetary perspective is being applied and on whether one believes that there is focus on the relevant utility generating components of the specific health care production.
Two concepts are important for ensuring overall efficiency: production and allocative efficiency. Production efficiency addresses the issue of using optimal combinations of resources to maximize health output. It is about choosing different combinations of resources to achieve the maximum output for a given cost. Allocative efficiency involves ensuring the right allocation of resources across programs such that the overall good is maximized. ‘Utility’ is an economic term, which measures the value/good of a produced outcome as perceived by the recipient. Utility-generating outcomes include factors beyond health outcomes, such as process utility or disutility and the value of information and choice. Alternatively, if allocative efficiency is defined more narrowly, it is about achieving the right mixture of healthcare programs in order to maximize the health of society.
Production Efficiency: Minimizing Cost Of Production
Production efficiency corresponds to accomplishing a job with minimum expenditure of time and effort. In the production of health care services, this can be translated into having an optimal combination of operating theaters and staff. If the hospital is understaffed, the operating theaters will not be utilized efficiently, and if there are too many staff members some will at times be redundant. In ensuring production efficiency, focus may be on improving staff ratios, shortening length of stay in hospitals, or eliminating unnecessary diagnostic procedures. An array of combinations of minimum input factors that can produce the same level of output are identified, and production efficiency is obtained by considering unit costs in order to determine which of the possible combinations of input factors minimizes overall costs. In the case that unit costs differ across regional health care authorities due to variations in the scarcity of specific resources (and thus opportunity costs), different combinations of input factors may represent production efficiency across regions. Some people will distinguish between technical efficiency (which focuses on the minimum amount of factors required for a specific level of output) and production efficiency (which in addition considers unit costs). For ease of presentation, no distinction is made between these concepts in the text that follows.
Allocative Efficiency: Determining What Should Be Produced
Allocative efficiency is about allocating resources such that the maximum utility is generated in terms of either health outcomes or a broader definition of utility-generating outcomes. An allocative efficient distribution may be Pareto efficient: A given distribution of resources that is not Pareto efficient implies that a certain change in allocation of goods may result in some individuals being made ‘better off’ with no individual being made worse off. A reallocation of resources can, therefore, improve overall welfare and a Pareto improvement is feasible. A less restrictive criterion for allocative efficiency is the Kaldor–Hicks efficiency, where an outcome is considered more efficient if those individuals that are made better off could in theory compensate those that are made worse off despite compensation not actually taking place.
Why Measuring Efficiency Is Pertinent In The Context Of Health Care
In theory the market for goods will automatically reach production and allocative efficiency if certain criteria are fulfilled. On the demand side, buyers in the market must be facing the full price of the good at the point of purchase and they must be able to make rational choices based on perfect and full information of the good. On the supply side, suppliers must be profit maximizers, there should be many competing suppliers, and there should not be factors deterring suppliers from moving easily in and out of the market.
In the market for health care services, these criteria are not fulfilled. First, there is a high degree of asymmetry of information, and those demanding health care services are not necessarily fully aware of which services they need, nor are they always able to judge the effectiveness of the services. Moreover, there is uncertainty regarding when the services are needed and how much they will cost. The economic uncertainty creates a market for health insurance, which means that the condition of the buyer facing the full price of the good is often not fulfilled. On the supply side, suppliers have been restricted from freely accessing the market in order to protect the less than perfectly informed patient/consumer. For example, doctors and other health care personnel have to be certified. Further, there has been a push for establishing nonprofit health care organizations on the market, again in order to protect the patient from profitseeking suppliers.
Hence, on the supply side there are factors, which undermine a competitive market and thus the mechanisms, which will ensure that health care services are produced at minimum cost. This means that production efficiency is not guaranteed. At the same time, consumers/patients are often not equipped to judge which health care services they require and are unlikely to face the full price at the time of purchase. This means that there is insufficient basis for ensuring allocative efficiency. Consequently, production efficiency and allocative efficiency are not guaranteed by market forces, and ensuring efficiency on the market for health care services is, therefore, an important issue for health care planners, politicians, and health economists.
Methods Of Measuring Efficiency In Health Care
Production and allocative efficiency are not independent concepts. Clearly, the unit of production that has to be maximized at minimum cost when focusing on production efficiency should be produced at the levels of quantity and quality that ensure allocative efficiency. In other words, one may be able to produce an inferior health care service very efficiently, but if there is no demand for the service, it is not worth bothering. Moreover, in ensuring a high level of production efficiency, one may be compromising allocative efficiency if the quality of the service is undermined when costs of production are reduced.
In the following are presented various methods of measuring production and allocative efficiency along with comments on the strengths and weaknesses of different methods.
Measuring Production Efficiency
Production efficiency entails producing the maximum output at a given level of employed resources. To measure and monitor production efficiency, it is essential to define the output produced as well as the production process that is under scrutiny. Outputs are typically measured in terms of services (hospital discharges, episodes of care, or covered lives) or in terms of health outcomes (postprocedure mortality rates, life expectancy, infant mortality rates, etc). There are two tools, which are typically applied in order to measure production efficiency in the context of production of health care services: productivity analysis and cost-effectiveness analysis (CEA). These will be described in turn in the paragraphs below.
Productivity analyses typically focus on an organizational unit’s ability to produce maximum output at minimum costs. The output measured is often the most obvious, i.e., number of treated patients or number of consultations. The cost is most often the cost to the organization (i.e., hospital costs). Productivity analyses are often used to benchmark hospitals or hospital departments in order to identify hospitals or hospital departments which demonstrate inefficiency in production.
The level of production efficiency of a particular hospital is characterized by the relationship between observed production and some ideal or potential production. The measurement of efficiency is based on deviations of observed output from the best production or efficient production frontier. If a hospital lies below the frontier, then it is inefficient, with the ratio of the actual to potential production defining the level of efficiency of the individual firm. There are two distinct methods for estimating production efficiency: parametric and nonparametric methods. Some general concerns and challenges in applying such methods should be mentioned. The cost of production is generally limited to that of the hospital or the hospital department and may, therefore, ignore other costs involved in the production process if these lie outside the organization which is analyzed. An observed improvement in production efficiency from this narrow perspective may, therefore, not necessarily reflect cost savings from a wider (societal) perspective. Moreover, the measure of output in productivity analyses is often reliant on available output measure such as number of patients discharged or number of hospital bed days. To the extent that these intermediate measures of output do not adequately reflect utility-generating outcomes, allocative efficiency may be compromised. This is especially the case if there are strong incentives to ensure cost savings, although the quality of services produced remains unmonitored. Recently, there is an increasing focus on refining productivity analyses by incorporating dimensions of quality in output (such as mortality and wound infections) in addition to number of hospital discharges.
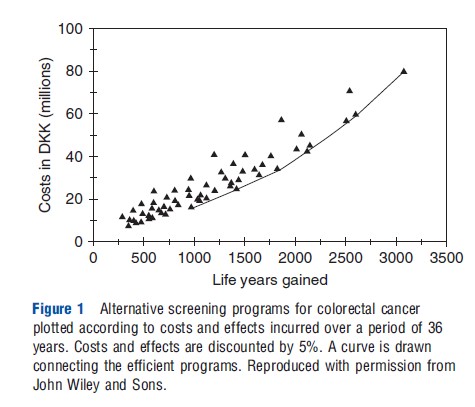
As in productivity analyses, CEA focus on comparing predefined outputs and comparing these with costs of production (where a perspective is chosen which may be more or less restrictive with respect to what cost items are included). If a CEA focuses on intermediate outcomes (such as numbers of cancers detected or reduction in blood pressure), the analysis is as restricted as a productivity analysis in the conclusions that can be drawn. Comparisons can only be made across interventions producing the narrowly defined unit of production, and only if an intervention is less effective and more costly or as costly as another intervention, can it be concluded that the former is inefficient. Note that for this type of CEA as well as for productivity analyses no conclusions can be drawn with respect to the relative merits of the efficient interventions (i.e., those interventions that lie on the production possibility frontier (PPF)). Figure 1 gives an example of such a frontier, where each triangle denotes a potential colorectal cancer screening strategy (target group and screening interval is varied) and the line represents the PPF (Gyrd-Hansen and colleagues, 1998). Program options that lie within the PPF are inefficient as they are dominated by at least one other program, which is either cheaper and/or more effective. Those programs that lie on the PPF represent programs that are technically efficient. However, which (if any) of these programs that fulfill the criteria for allocative efficiency is undetermined.
CEA can be applied as a tool for guiding resource allocations across the health care sector as a whole. In this case, the production unit is either defined in terms of the health care sector or society as a whole and the output of interest is quality of life years (QALYs) gained. The broader definition of output ensures that CEA can guide the allocation of resources across various types of health care interventions aimed at different patient groups. The key parameter in this case is the cost per QALY, also referred to as the incremental cost-effectiveness ratio (ICER). Many health economists would define CEA applied in this way as a tool for ensuring production efficiency within the health care sector, i.e., ensuring that the maximum amount of output (QALYs) is produced at a given level of cost (given by the health care budget constraint). Other health economists perceive that we are in essence dealing with issues of allocative efficiency (within the bounds of the health care sector), where the aim is to ensure the optimal allocation of resources across services in the health care sector, and the maximization of QALYs is equivalent to maximizing benefits. Clearly, any disagreement on how the role of CEA is best defined is a matter of whether one defines allocative efficiency as necessarily meaning the allocation of resources across society as a whole or whether one can accept QALYs as a sufficient measure of benefits.
A more pertinent question is how CEA and ICERs are used in practice to inform decision making. In the ideal and very unrealistic scenario where all candidate health care interventions are subjected to economic evaluation and only those which are most cost effective (i.e., those with lowest ICERs) are included in the health insurance package subject to the given budget constraint, the CEA can fulfill the role of ensuring efficiency. In the more realistic scenario where resources are currently being used to run existing health care services, and there is only information on the ICER of a new intervention, the usefulness of the cost-effectiveness information is likely to be reduced. If the new health care intervention is cost saving or cost neutral, but more effective than the present intervention, the decision is straightforward. The intervention should clearly replace current practice. And vice versa if the intervention is cost neutral or cost generating and less effective. However, in many cases, new interventions are cost generating as well as more effective. In this case, it is not easy to draw any conclusions as to the welfare implications of introducing the new intervention. Introduction of the new intervention will necessarily incur opportunity costs in terms of health foregone, as there will be fewer resources available for other activities. It cannot be determined whether the health benefits foregone are larger or smaller than the acquired health benefits. Only if the health care services that may be deferred can be identified and evaluated, can an informed decision be made.
To improve the usefulness of ICERs as a tool for decision making, researchers have sought to identify a cost-per-QALY threshold as an indicator of whether an intervention is sufficiently cost-effective to warrant implementation. However, such a threshold is of little use as long as the true opportunity costs remain unidentified, which is likely to be the case if decisions are made under a predetermined budget constraint. Thresholds, as produced by way of a citizen’s WTP (out of own pocket) per QALY, are only useful instruments so long as the introduction of new interventions that pass the threshold requirements are facilitated through expansion of the health care budget, thus incurring opportunity losses from reduced private consumption.
QALY league tables rank (candidate) health care interventions according to their cost-effectiveness (cost per QALY). Such tables can be useful to identify whether efficiency could be improved if some interventions take the place of others, but this necessitates the inclusion of both existing and new interventions. The more exhaustive a QALY league table is, the more useful it can be as a means of improving overall allocation of resources. However, in presenting ICERs in QALY league tables, or elsewhere, it is important that the ICERs presented are those that most precisely reflect the cost-effectiveness of the given policy relevant choice. In many cases, it is not only a question of whether or not to implement a health care service but also of how to implement it and to whom it should be offered. Interventions such as neonatal care, screening programs for cancers, prophylactic treatment of high blood pressure, etc. can be designed in many ways. Offering a health care intervention to all may appear reasonably cost-effective on the basis of the average cost per QALY. The average value may, however, hide some very expensive QALYs if a specific group of recipients experience little health gain at a high cost. It is important to choose the right comparator, and the corresponding ICER, in order to appropriately inform on efficiency implications.
Measuring Allocative Efficiency
Measuring allocative efficiency is about determining which aspects of health care services are of value to citizens, and to determine the relative importance of health care services. Measuring allocative efficiency must, therefore, in principle involve consumer preferences . In CEA, allocative efficiency (more frequently labeled production efficiency) within the bounds of the health sector is obtained by measuring benefits in terms of QALYs. Although quality adjustments are to some extent based on consumer preferences , it has been argued that this measure of benefit may in some cases be too restrictive because it does not include other utility-generating aspects of health care services such as process disutility or the value of information. Although such factors are not present in all contexts, ignoring these may result in some degree of inoptimal resource allocation.
A guide to efficient resource allocation is cost–benefit analysis. Cost–benefit analysis is based on the Kaldor–Hicks criterion, where an outcome is more efficient if those that are made better off could in theory compensate those that are made worse off. In the case of a publicly funded health care service, the losers would be the taxpayers who are financing the service and the winners are those citizens who can expect to receive the service, should they need it. Assuming that individuals are rational and fully informed about the quality of a good, consumers will be willing to pay equivalent to the marginal utility that they anticipate from buying the good. Allocative efficiency is obtained when goods in society are produced at a level where price is equal to marginal cost. Cost–benefit analysis seeks to replicate the demand side of the market by using market observations (revealed preferences studies) or laboratory experiments (typically contingent valuation studies or discrete choice experiments) to establish consumers’ WTP for health care services.
Contingent valuation methods and discrete choice experiments typically involve asking people how much they are willing to forego (out of their private budget) in order to ensure access to a health care service. If a cost–benefit analysis demonstrates that WTP is higher than costs, this implies that allocative efficiency is improved if the health care service is introduced. For this conclusion to hold, additional resources must be taken from private funds. If it is instead a question of determining resource allocations within a predetermined health care budget constraint, it is necessary to evaluate all the specific programs that are competing for funds. Allocative efficiency (within the health care sector) is attained when the last dollar invested across all areas of health care services generate the same level of marginal utility.
One advantage of the cost–benefit approach is that it in principle can guide resource allocations across various sectors of society. Where CEA seeks to prioritize health care services within a given budget restriction, cost–benefit analysis could ideally indicate the size of the health care budget. The benefit measure used in cost–benefit analysis also has the advantage that it is broader and far less predetermined than the benefit measures in CEA. It rests on the notion that all preferences count, which necessarily opens up for a discussion of whether the goal of the health care sector is to serve needs or wants. The Achilles’ heel of cost-benefit analysis in the context of health care is whether rational and robust preferences based on a full understanding of the merits of the health care services can be derived. More research into how best to ensure that respondents understand and adequately respond to the information that is provided to them is warranted. Also, measures of allocative efficiency, which rely on private interests only, may neglect to incorporate societal benefits that are not reflected in preferences of the consumers (externalities).
To the extent that there are significant positive or negative externalities involved when providing a health care service (e.g., herd immunity), these should be valued and included in the cost–benefits analysis. The extension of allocative efficiency to encompass externalities is sometimes called social efficiency.
References:
- Boadway, R. and Bruce, N. (1984). Welfare economics. Oxford: Basil Blackwell.
- Culyer, A. J. (1989). The normative economics of health care finance and provision. Oxford Review of Economic Policy 5(1), 34–58.
- Donaldson, C., Currie, G. and Mitton, C. (2002). Cost effectiveness analysis in health care: Contraindications. British Medical Journal 325, 891–894.
- Gerard, K. and Mooney, G. (1993). QALY league tables: Handle with care. Health Economics 2(1), 59–64.
- Hicks, J. (1939). The foundation of welfare economics. Economic Journal 49, 696–712.
- Hollingworth, B. (2003). Non-parametric and parametric applications measuring efficiency in health care. Health Care Management Science 6(4), 203–218.
- McKay, N. L. and Deily, M. E. (2008). Cost inefficiency and hospital health outcomes. Health Economics 17(7), 833–848.
- Olsen, J. A. and Smith, R. (2001). Theory versus practice: A review of ‘willingness-to-pay’ in health and health care. Health Economics 10, 39–52.
- Salkeld, G., Quine, S. and Cameron, I. (2004). What constitutes success in preventive health care? A case study in assessing the benefits of hip protectors. Social Science & Medicine 59, 1593–1601.