Why Do Sex Workers Engage In Noncondom Use?
Much of the health policy literature argues that in many cases sex workers engage in unprotected sex because they are uninformed of the risks and that they would protect themselves if they fully understood the risks (World Bank, 1999; Lau et al., 2002). In the cases in which sex workers are aware of the risk, others hypothesize that noncondom use occurs because condoms are either very expensive or not available at all (Negroni et al., 2002), implying there are serious supply-side constraints. Alternatively, others have argued that sex workers are forced to have unprotected sex (Karim et al., 1995; World Bank, 1999), and because they face physical or economic threats, they engage in noncondom use.
Although ignorance does exist and the forced exploitation of sex workers does occur, another possible explanation is that sex workers are willing to risk infection by not using condoms with clients if they are adequately compensated. Indeed, economic theory has long posited the general principle of compensating wage differentials (Rosen, 1986), and a number of authors have documented wage differentials that compensate for risky work activities in other labor sectors such as mining, police work, and firefighting (Viscusi, 1992; Siebert and Wei, 1998). Although there is anecdotal evidence that sex workers charge more for sex without a condom (Ahlburg and Jensen, 1998), there was little empirical evidence testing this claim before research from the economics community. In addition, it has been widely documented that men have strong preferences for noncondom sex. Therefore, if men are willing to pay more for sex without a condom, then sex workers might simply respond to these market incentives.
Understanding why sex workers do not use condoms is critical for the development of policy that is effective in increasing condom use and consequently in reducing the transmission of STIs, including HIV. The usual policy recommendations are to intervene on the supply side (World Bank, 1999). These policies include (1) educating sex workers about the risks, (2) increasing access to inexpensive condoms, (3) reducing environmental barriers to condom use by working with gatekeepers such as brothel owners and the police, and/or (4) empowering sex workers by improving their negotiating skills and fostering self-help organizations. Additionally, governments are urged to implement and enforce laws against human trafficking, rape, assault, and indentured servitude. However, if some clients are willing to pay substantially larger sums for unprotected sex, supply-side interventions alone are less likely to sufficiently reduce unprotected commercial sex. Even knowledgeable sex workers with condoms, who are free to turn down clients, might be willing to supply unprotected sex if the price is right. In this case, complementary interventions on the client side that reduce the demand for unprotected sex are also necessary in order to increase condom use.
Gertler et al. (2005) investigate whether sex workers are rationally responding to market incentives by testing whether sex workers charge more to take the risk of providing unprotected services. However, selection is an issue due to both sex worker heterogeneity as well as client sorting. For example, in terms of sex worker heterogeneity, better educated sex workers might charge higher prices and also be more likely to use condoms. Similarly, better educated, wealthier clients who value condom use and have a higher willingness to pay may select these sex workers. This will create a positive correlation between price and condom use, which is not necessarily causal or related to compensation for taking a risk. To control for the endogeneity of condom use, they collect information on the last 3–4 transactions for each sex worker to create a panel dataset. They estimate a model with sex worker fixed effects to control for bias from both unobserved sex worker heterogeneity and client selection where the dependent variable is log price. Additionally, they control for client characteristics using sex worker reports of clients’ looks, wealth, cleanliness, and risk preferences.
Gertler et al. (2005) begin by constructing a simple bargaining model of commercial sex that has a number of empirically testable predictions. The model predicts that a condom will not be used when the client’s maximum willingness to pay not to use a condom is greater than the minimum the sex worker is willing to accept to take the risk. Surprisingly, however, the model also predicts that when the client is worried about the risk of infection from unprotected sex, he may be charged more for using a condom than for unprotected sex. Similarly, when the sex worker prefers not to use a condom, the client is given a discount for not using a condom. The price differential between protected and unprotected sex is a weighted average of the maximum the client is willing to pay for not using a condom and the minimum the sex worker is willing to accept to take the risk of infection by not using a condom. The weights are a function of the relative bargaining power of the client and the sex worker.
Gertler et al. (2005) test these predictions using a panel dataset collected in 2003 from the Mexican states of Michoacan and Morelos. They find that Mexican sex workers receive a 23% premium for unprotected sex from clients who requested not to use a condom, and this premium jumps to 46% if the sex worker is considered very attractive. They also find that clients who requested condom use paid 9% more for protected sex, and sex workers who requested not to use a condom gave clients a 20% discount. The results are completely consistent with the theoretical predictions.
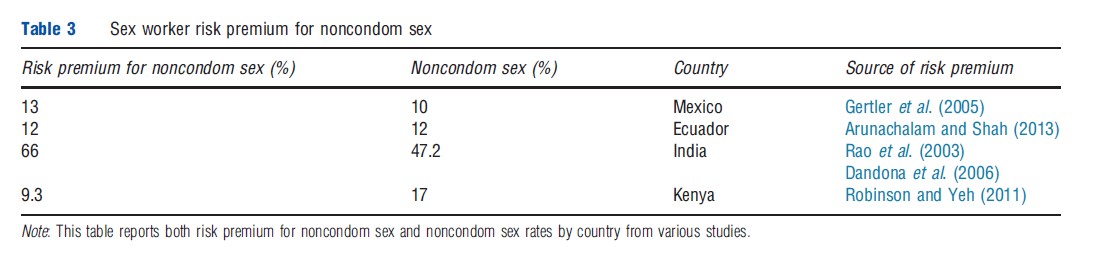
Studies in other developing countries have found similar results with male clients paying a premium for noncondom use in India (Rao et al., 2003), Ecuador (Arunachalam and Shah, 2013), and Kenya (Robinson and Yeh, 2011). Table 3 summarizes the main results from all these studies. Arunachalam and Shah (2013) and Robinson and Yeh (2011) use a similar sex worker fixed effects empirical strategy as Gertler et al. (2005).
Interestingly, Arunachalam and Shah (2013) show that the premium men pay for noncondom sex in Ecuador is approximately 12% but that this premium increases in locations with higher disease rates. A one percentage point increase in the local STI rate increases the premium for noncondom sex by 33%. This is the first paper in this literature to have biological STI outcomes for sex workers. Therefore, the authors are able to identify this source of the risk premium as directly linked to STI rates. These results suggest that market forces may curb the self-limiting nature of STI epidemics exacerbating the spread of disease. To a greater extent than other epidemics, economists argue that the spread of STIs is shaped by individuals’ behavioral responses. For example, with an increase in awareness of the risk of contracting disease, individuals substitute away from risky sex toward abstinence (Kremer, 1996), toward protected sex (Ahituv et al., 1996; Dupas, 2011), or away from sex with men toward sex with women (Francis, 2008). Viewing risky sex much like other commodities in the market, economists anticipate that demand declines as the expected cost increases (Posner, 1992). Hence, economists tend to see behavioral responses to STI prevalence as generating a self-limiting incentive effect of epidemics (Geoffard and Philipson, 1996). Evidence from the commercial sex sector, however, suggests that market forces may dampen the self-limiting feature of STI epidemics be cause sex workers draw a premium for engaging in risky unprotected sex.
Robinson and Yeh (2011) use a panel dataset constructed from 192 self-reported diaries of women who provide transactional sex in Busia, Kenya. They find that women who engage in transactional sex increase their supply of risky, better compensated sex to cope with unexpected health shocks, particularly when another household member is ill. More specifically, they find that women are 3.1% more likely to see a client, 21.2% more likely to have anal sex, and 19.1% more likely to engage in unprotected sex on days in which another household member (typically a child) falls ill. These behavioral responses obviously entail significant health risks for these women and their partners, and suggest that women are unable to cope with risk through other consumption smoothing mechanisms. This is an extremely critical issue in a place like Busia, where the estimated HIV prevalence was 9.8% in 2004 (CBS, 2004).
In India, Rao et al. (2003) use 2003 data from Songachi, Kolkata’s oldest and best established red-light district, with more than 4000 sex workers working in 370 brothels that service approximately 20 000 clients a day. Rao et al. (2003) use an instrumental variable strategy to estimate the premium for noncondom sex and correct for unobserved heterogeneity. They use exposure to an HIV/AIDS intervention targeted at sex workers as the instrument because this intervention is highly correlated with a sex worker’s propensity to use condoms, but the authors claim it is uncorrelated with a sex worker’s income. They estimate that when sex workers use condoms, they earn between 66% and 79% less.
The loss in earnings associated with condom use clearly represents a major disincentive to safe sex. The problem comes from the fact that clients, most of whom do not want to use condoms, are able to exploit competition among sex workers. If a sex worker insists on having sex with a condom, the client can simply go to the next brothel or another sex worker in the same location where he will find a sex worker who is more willing. The solution to this can come either from educating clients about safe sex or creating an agreement among sex workers to collectively agree to refuse condom-free sex (Rao and Shah, 2012).